Froedtert & the Medical College of Wisconsin - Liver Cancer Minimally Invasive Therapies
About our Therapies
Local Ablation
Physicians in the Liver Cancer Program use a variety of minimally invasive treatments for destroying liver tumors using heat or cold energy. These local ablation procedures are typically used to treat well defined small tumors that cannot be surgically removed.
- Radiofrequency ablation (RFA): Using ultrasound or CT guidance, an electrode-tipped probe is positioned inside the liver tumor. A radiofrequency current is then passed through the electrode, creating energy that destroys (or ablates) the tumor tissue near the probe tip. The energy also closes small blood vessels, minimizing the risk of bleeding.
- Cryoablation: This procedure uses cold energy to freeze and destroy tumor tissue. The probe is positioned within the tumor using imaging guidance and cooled to -190° C (-360° F), engulfing the tumor within an ice ball and resulting in the death of tumor cells. The physician can easily monitor the margins of the ice ball with ultrasound or CT imaging and adjust the probe output as needed. Because of this ability to monitor and control the ablation zone, cryoablation can be used to treat tumors that are close to critical structures.
- Microwave ablation: Liver tumors that are adjacent to a large blood vessel can be difficult to treat with RFA and cryoablation. The large volume of blood flowing past the ablation zone tends to cool (or warm) tumor tissues, preventing them from sustaining cancer-killing temperatures. Microwave ablation technology achieves higher temperatures more quickly than other options, which facilitates treatment of tumors near large vessels.
RFA, microwave and cryoablation can also be performed during liver surgery. To find out more, visit our liver cancer surgery section.
Interventional Radiology Techniques
Systemic treatments like chemotherapy expose the entire body to cancer drugs, leading to side effects and limiting the dose of drug that can be delivered to the tumor. Several interventional radiology (IR) techniques are available for delivering drugs and other therapies exclusively to the region affected by the cancer. These therapies can be effective options for patients with large liver tumors or extensive liver cancer, provided the patient’s ability to function in normal daily routines, and his or her liver function are both acceptable.
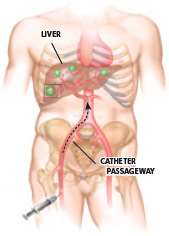
- Chemoembolization is a method for delivering chemotherapy directly into a tumor. A catheter is placed in a groin artery and guided into the branch of the hepatic artery that supplies blood to the cancer tissue. In a standard chemoembolization procedure, a potent dose of a chemotherapy drug mixed with oil is infused through the catheter to the tumor. Embolization particles are then injected into the artery, trapping the drug at the cancer site and blocking tumor blood flow. The tumor receives a very high dose of chemotherapy with minimal systemic side effects for the patient. Alternative chemoembolization techniques use embolization beads that are themselves loaded with the chemotherapy drug. These drug-eluting beads allow for a slow release of the cancer drug over a long period, which may lead to fewer systemic side effects. Patients may undergo chemoembolization multiple times if needed.
- Radioembolization procedures deliver radiation directly to liver tumors in the form of microscopic beads impregnated with radioactive yttrium-90. In an outpatient procedure, a catheter is placed into the femoral artery at the groin and guided to the branch of the hepatic artery that feeds the tumor. Radioembolization beads are then infused through the catheter into the artery. The spheres become lodged in the small blood vessels that feed the tumor, delivering radiation to the cancer site with minimal effect on surrounding healthy tissues.
Local therapies can be important for patients who are waiting for a liver transplant. The criteria for transplant are strict, and patients whose tumors grow too large can become ineligible for a transplant operation. For these patients, embolization or ablation can serve as a “bridge therapy” — preventing tumors from progressing while the patient is on the transplant waiting list. For some patients who are just outside transplant criteria, regional therapies are sometimes able to shrink a tumor, thereby making the patient eligible for a transplant procedure.
To learn more about embolization and other regional therapies, visit our Regional Cancer Therapy Program section.
Portal Vein Embolization
Surgeons can remove up to 80 percent of the liver and it will grow back in a matter of weeks provided the liver is healthy. Nonetheless, some patients do not have enough healthy liver tissue to enable an extensive resection. For these patients, an IR procedure called portal vein embolization (PVE) can make surgery possible by increasing the volume of healthy liver.
PVE is performed several weeks before the planned liver surgery. Using catheter-based tools, an interventional radiologist blocks the branch of the portal vein that supplies blood to the side of the liver planned for removal. This causes the other side of the liver to grow larger. In patients who do not have underlying liver disease, the healthy part of the liver will grow enough in several weeks to make surgery possible. Patients with less than 30 percent healthy liver usually undergo PVE before surgery to increase their remnant liver volume.
Stenting Procedures
Liver tumors can block bile ducts within the liver. This can lead to pain and other complications. For these patients, interventional radiologists can insert wire mesh stents in ducts to relieve tumor pressure. Relieving blockage can help restore liver function, enabling patients to tolerate chemotherapy.