MCW Pain Medicine Team Investigates Use of Virtual Reality for Pain Management

Amid the quest for comprehensive pain management strategies, virtual reality (VR) emerges as a promising nonpharmacological intervention. Prior studies have demonstrated its efficacy in alleviating pain across various clinical conditions. The mechanism involves sensory immersion, limiting attention to injury-related pain, and reducing visual cues that amplify anxiety in medical environments.
Sarah Trost, PhD, assistant professor and pain psychologist at the Medical College of Wisconsin (MCW), believes VR could potentially be a useful tool in managing chronic pain. Together with her colleagues in the Department of Anesthesiology, Amit Singh, DO, Lisa Elliott, APNP, Sarah Endrizzi, MD, and Rebecca Anderson, PhD, the team’s interest in VR stemmed from a desire to offer alternative nonopioid treatments for patients dealing with persistent pain. This exploration was fueled by collaboration with David Chao at Inception Health, who provided the necessary VR unit in partnership with Applied VR.
"Anytime that you can find a nonopioid treatment that's going to make someone's life a little bit better in the hospital, we're excited about that," Dr. Trost says.
The research was structured as a pilot study with the primary objective of assessing the feasibility and effectiveness of VR as a tool for pain management. The study targeted inpatients experiencing various types of pain, including musculoskeletal and postsurgical pain. Patient autonomy was a key element, allowing individuals to choose from a range of VR programs, each offering distinct immersive experiences.
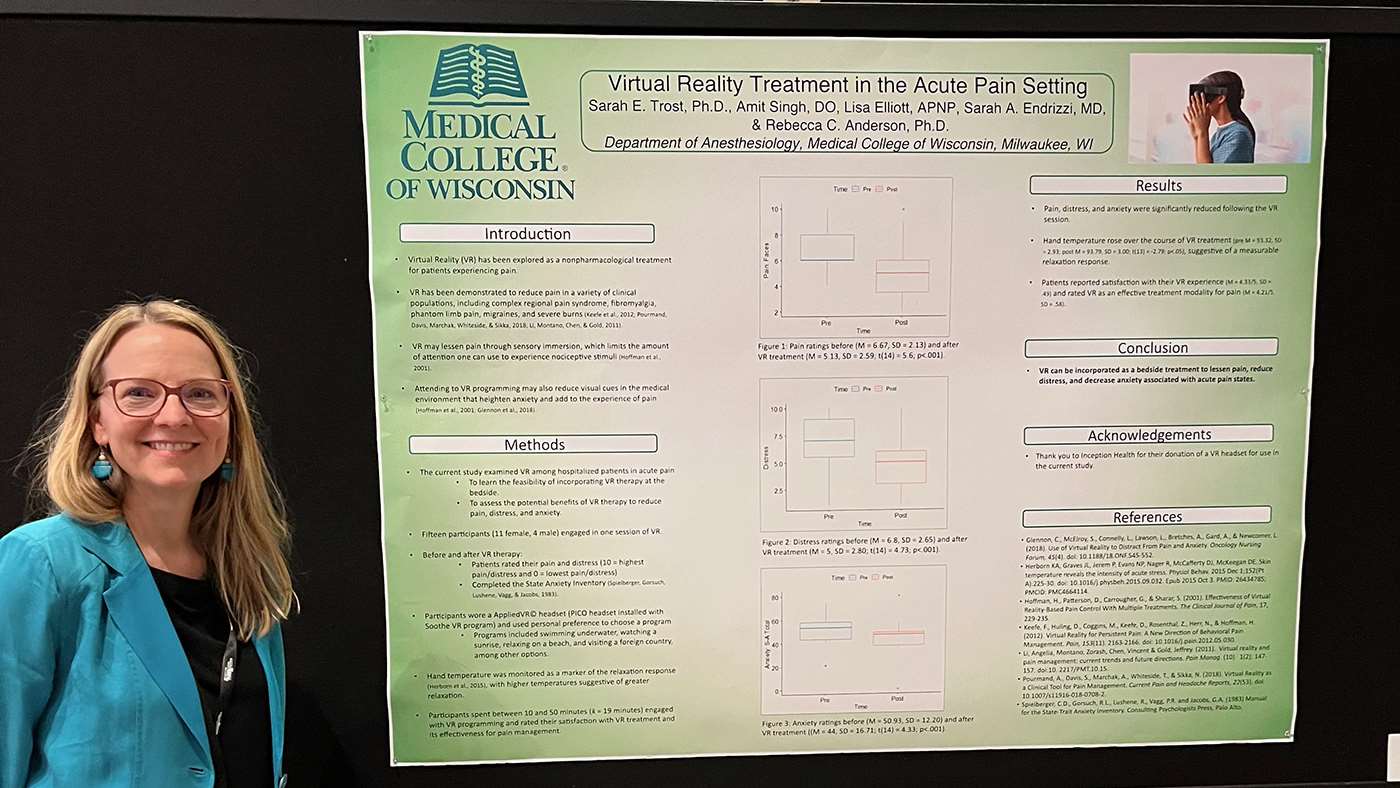
Fifteen participants (11 female, 4 male) engaged in a single VR session, selecting programs such as underwater swimming or beach relaxation. Pain and distress were rated on a 10-point Likert scale, and the State Anxiety Inventory measured anxiety. Hand temperature served as a marker of the relaxation response. Participants spent 10-50 minutes, 19 minutes on average, in VR, and satisfaction and effectiveness were self-assessed.
Patients' experiences were measured by changes in pain and distress levels before and after engaging in VR sessions. Data showed significant reductions in pain, distress and anxiety for nearly all participants. The research team also observed anecdotal evidence suggesting positive outcomes, with patients expressing satisfaction and relief. This study demonstrates the feasibility and efficacy of incorporating VR as a bedside treatment to reduce pain, distress and anxiety in hospitalized patients experiencing acute pain.
 Lisa Elliott (pictured right) helped identify the patients who were candidates for the study and oversaw the patients’ sessions. Elliott noticed a positive change in the participants as soon as they began using the VR headsets. “It was incredible to see how patients were finally able to relax and smile as soon as they slipped the goggles on,” Elliott says. “For a brief period of time, they were able to escape the sights and sounds of the hospital and fully immerse themselves in the virtual landscape of their choosing.”
Lisa Elliott (pictured right) helped identify the patients who were candidates for the study and oversaw the patients’ sessions. Elliott noticed a positive change in the participants as soon as they began using the VR headsets. “It was incredible to see how patients were finally able to relax and smile as soon as they slipped the goggles on,” Elliott says. “For a brief period of time, they were able to escape the sights and sounds of the hospital and fully immerse themselves in the virtual landscape of their choosing.”
"It truly is an immersive experience, and that's a key factor in the effectiveness of VR. Being fully engaged in an environment helps minimize the impact of visual cues from the medical surroundings," Dr. Trost says. "Through this sensory immersion, individuals may find themselves less attentive to pain sensations."
Collaboration with Inception Health and Applied VR facilitated access to cutting-edge technology, contributing to the success of the research. The team's use of VR aimed to alleviate pain, distress and anxiety, presenting a nonpharmacological approach to patient care.
Looking ahead, the team express enthusiasm about extending the use of VR to other hospital settings, perhaps to support post-surgical outcomes. In addition, they are considering how to incorporate VR into outpatient settings. This strategic expansion aligns with the overarching goal of enhancing patient care and well-being.
“I think distraction and immersive relaxation techniques are underutilized,” Elliott says. “My hope is that we can continue to incorporate these kinds of strategies in both the inpatient and outpatient settings in the future.”