Milwaukee (MKE) Residency Program at the Medical College of Wisconsin
The MCW-MKE Psychiatry Residency program is a long-established program in the fantastic city of Milwaukee. We have a unique curriculum that we believe maximizes the breadth and depth of experiences. The MKE psychiatry program is home to all of the available ACGME fellowships, including Addiction Psychiatry, Child & Adolescent Psychiatry, Consultation-Liaison Psychiatry, Forensic Psychiatry and Geriatric Psychiatry.
A message from our Residency Program Director
Combined Internal Medicine/Psychiatry Program
Program Overview
Different than most programs that offer ambulatory psychiatry in the PGY 3 year, our outpatient clinic begins in second year of training with continuing psychotherapy clinics throughout the rest of residency.
This unique curriculum allows residents to have continuity with patients for several years. It also allows residents to build on the knowledge, skills and perspective learned in outpatient psychiatry when they return to the inpatient, emergency and consultation liaison settings in the third year, enhancing the PGY 3 experience. Third year inpatient rotations add the dimension of group psychotherapy, while fourth year is rounded out with neurology, integrated care, psychotherapy and electives.
Our program is fortunate to work with multiple health systems in the Milwaukee area to give residents an experience in a diverse range of settings – from a VA hospital to private psychiatric hospitals to an academic medical center. Residents rotate at the new Mental Health Emergency Center (MHEC) – a busy psychiatric emergency room opened in 2022 as a joint venture between Milwaukee County and four local health systems to serve residents of the state’s most populated county. Second year residents spend half of their time in our free-standing psychotherapy center where they learn supportive psychotherapy, psychodynamic psychotherapy and cognitive behavioral therapy.
Consultation-liaison (CL) psychiatry is another area of strength with residents doing five months of CL, including one at the Children’s Hospital of Wisconsin. Fourth year residents carry on their CL experience in the outpatient setting, serving as consultants in one of our integrated care clinics. The consultation clinics span the range of integrated care, from co-located care in the Perinatal Clinic to a public health approach with care coordinators in several of our Primary Care Clinics.
I specifically ranked this program as #1 over several Ivy League programs because MCW Psychiatry is about learning and takes a very holistic approach to fostering its learners which shows in every aspect of the program and the opportunities we receive.
A "Day in the Life"
Program Information
Contact Us
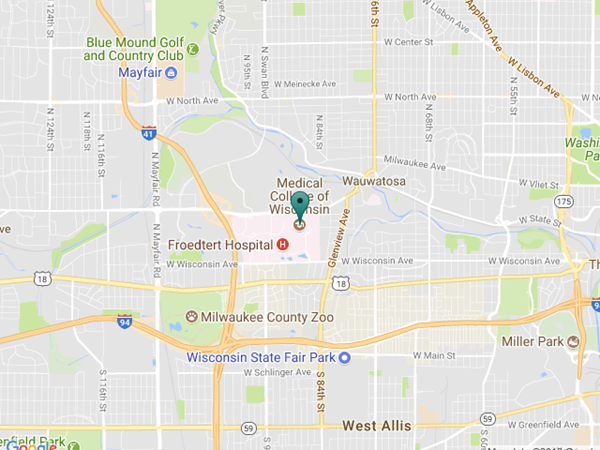
Physical Address
Psychiatry and Behavioral Medicine
Tosa Health Center
1155 N. Mayfair Rd., Third Floor
Milwaukee, WI 53226
Mailing Address
MCWAH Psychiatry Residency Program – Milwaukee
8701 Watertown Plank Rd.
Milwaukee, WI 53226
(414) 955-8998
(414) 955-6585 (fax)