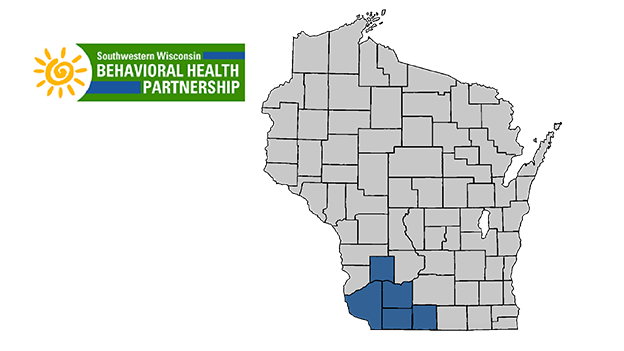
Southwestern Wisconsin Behavioral Health Partnership (SWBHP) - Grant, Green, Iowa, Lafayette & Richland Counties
Impact
After forming, the partnership soon realized they needed a broad focus to truly improve access to care. This meant both focusing on the larger community factors that uphold barriers to access and improving the levels of acceptability and availability of mental health care in the region.
Stigma is one of the most commonly cited reasons for not seeking treatment. The lack of privacy and cultural attitudes surrounding mental healthcare in rural communities creates social distancing and increases barriers that can detract from efforts to increase services that address stigma. These facts influenced SWBHP’s aim to bring broad cultural change by improving knowledge about stigma, with the ultimate goal of building a community that supports training, education, and dialogue – a community unafraid to seek help when it’s needed.
To reinforce this effort and increase the availability of care, the partnership also worked to offer community members and peers supporters trainings on mental health intervention, giving them the necessary knowledge and resources to provide early, but crucial levels of care.
SWBHP’s multi-county system for collaboration included individuals from a wide variety of sectors. Community members with lived experience, peer support specialists, and community outreach leaders provided personal perspectives, while healthcare professionals from primary care providers, mental and behavioral health providers, and community outreach staff contributed their expertise to the partnership. Additionally, leadership from local schools, higher education, local and county law enforcement, health and human services, aging and disability organizations, faith-based organizations, and more across all five counties were included to develop accessible systems for collaboration between counties to increase resources needed to confront and reduce poor mental health.
Normalizing Discussions around Mental Health and Seeking Treatment
Improving the Navigation Systems to Access Resources
Increase Community Support for Each Other
Highlights/Select Work Product
- Southwestern Wisconsin Behavioral Health Partnership's Network of Care Southwestern Wisconsin Network of Care - Serving Grant, Green, Iowa, Lafayette and Richland Counties, Wisconsin
- Asset Mapping and Community Development
- Mental Health Crisis Intervention Team
- Break Your Stress Cycle
- Advancing Behavioral Health in Southwestern Wisconsin
County-level Mental Health Volunteer Groups:
Annual Mental Health Summit held in 2018, 2019, 2021, 2022 & 2023:
- 2019 Summit Program (PDF)