Adaptive Optics (AO) in the MCW AOIP
Human Adaptive Optics Imaging
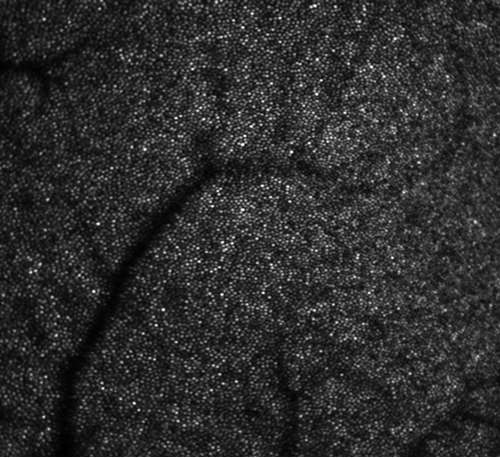
The AOIP has a robust human adaptive optics imaging program, with volunteers coming in daily for a variety of studies. We have two AO scanning light ophthalmoscope systems designed by the Dubra lab and optimized for human imaging, each with unique advantages for gathering data on photoreceptors, vasculature, and nerve fiber layers of the retina.
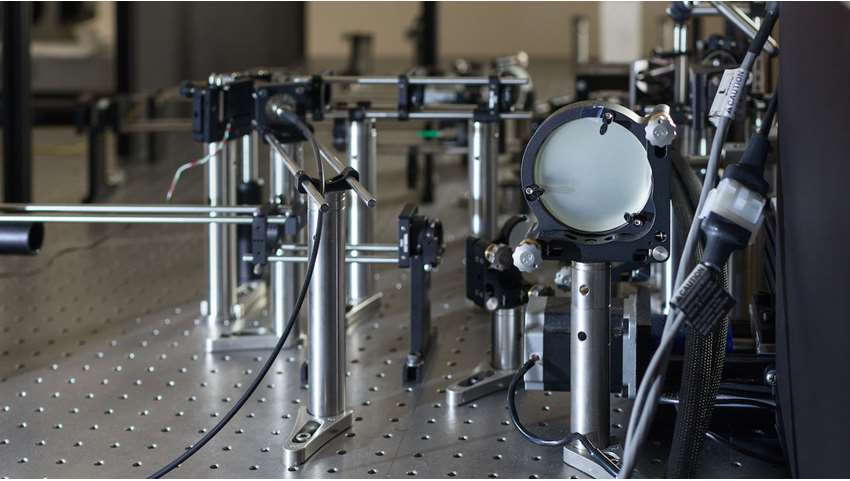
One system was designed with a maximized pupil size for high resolution of individual photoreceptors, while the other has a smaller pupil size optimized for widefield imaging and makes it possible to image volunteers with restricted pupil sizes.
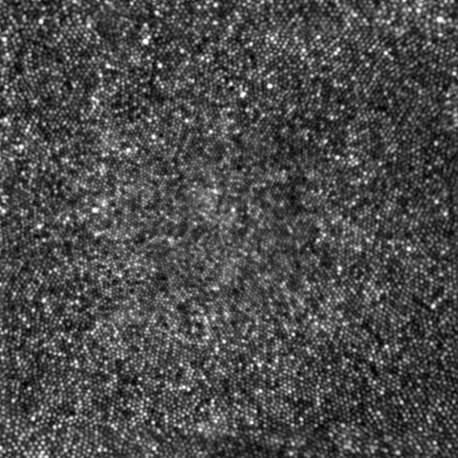
Our lab has focused on using AOSLO imaging to better understand retinal diseases and conditions in an effort to inform treatment development. We have described retinal morphology in healthy retinae as well as retinae affected by conditions such as achromatopsia (Langlo et al. 2016), retinitis pigmentosa (Sun et al. 2016), albinism (Wilk et al. 2017), color vision deficiencies (Patterson et al. 2018), and macular telangiectasia (Litts et al. 2020). Much of our research has also focused on the evaluation of disease biomarkers and progression that cannot be observed without the high resolution of adaptive optics (Litts et al. 2017).
A new avenue of research at the AOIP involves better understanding how vision and retinal structure recover following retinal trauma. Clinical tools available today are not always able to capture pathological changes to retinal structure during the process of recovery – giving the appearance of healthy retinal structure although there are disruptions to vision still present. By combining the use of AOSLO with various clinical tools, we can compare the results and explore ways to detect subtle differences in retinal structure clinically. At the AOIP, we are exploring how photoreceptors recover both structurally and functionally from different conditions in animal models as well.
One current AOSLO-based study is a new collaboration with the VA hospital to examine the effect of traumatic brain injuries (TBI) on retinal structure and function. Many patients with a history of TBI experience visual system dysfunction but lack clinical findings that would suggest a retinal cause. AOSLO imaging has revealed disruptions to the photoreceptor mosaic following TBI that went undetected by clinical structural imaging (Braza 2018, Scoles 2016, Flatter 2014). At the AOIP, we are investigating whether these subtle changes to the photoreceptor mosaic contribute to visual dysfunction following TBI using AOSLO and OCT.
We are also exploring the changes in macular structure following macular hole repair using AOSLO and clinical tools. Visual outcome following macular hole repair is variable, both in terms of timeline for recovery and the amount of improvement in vision. At the AOIP, we believe this variability relates to the severity of photoreceptor damage and amount of photoreceptor recovery. We have previously shown that photoreceptor structure recovers over time following macular hole closure (Hansen 2015). Data collected from this population also supports the hypothesis that photoreceptors are capable of regeneration and are more likely to recover function over cell migration to injured retinal locations (Hansen 2015, Randerson 2015). We hope to explore this topic in many different people recovering from macular hole surgery to better understand the process of photoreceptor recovery.
The AOIP is collaborating with Dr. Berge Minassian from the University of Texas Southwestern Medical Center to explore the retinal changes associated with Lafora Disease and Adult Polyglucosan Body Disease. These are neurodegenerative metabolic diseases that lead to the accumulation of insoluble, faulty glycogen (called polyglucosan aggregates) molecules throughout the body. Within the eye, inner retinal cells, which act like telephone wires sending visual information from photoreceptors to the brain, are negatively affected by polyglucosan aggregates. We are using AOSLO to explore inner retinal phenotypes associated with these diseases with the goal of identifying retinal biomarkers of neurodegenerative disease. Retinal imaging is time and cost effective for patients when compared to brain imaging. Identifying retinal markers of neurological disease would improve how we diagnose and manage these conditions.
The AOIP also conducts AOSLO imaging for companies developing treatments for retinal diseases, such as gene therapies for inherited conditions such as achromatopsia and X-linked retinitis pigmentosa. Our images and analysis provide detail on how the treatments affect the retina at a cellular level, providing insight on their risks and efficacy.
If you are interested in talking to one of our lab members or joining us, see our People page for contact information. If you would like to collaborate, please visit our Collaboration page. See our publications page for a complete list and links to our published works.