MCW Emergency Medicine Residency Curriculum
EM Curriculum Details
EM Simulation Curriculum
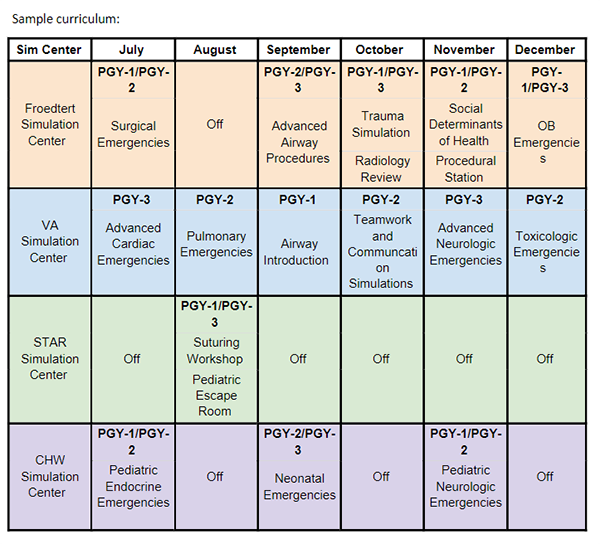
The resident simulation curriculum is designed to give residents exposure to a variety of cases, procedures, and emergency medicine skills to help develop their clinical practice.
The current simulation curriculum spans the 12-month academic year with a dedicated conference day each month. Our simulation days utilize the four simulation centers listed above, with residents splitting up between 2-3 sites each month. This allows small groups of 3-6 learners per simulation and maximize hands-on experience. The curriculum is designed to target residents’ specific skill levels during training with escalation of roles and advanced skills each year.
In addition, the simulation team collaborates with other departments, including emergency medical services, neonatology, obstetrics and gynecology, trauma surgery, and neurology, to provide interprofessional scenarios for residents.
Finally, with a large simulation staff and multiple training centers, residents can experience simulation “on the other side” with the developing and running simulation cases if they are interested in learning more.
EM Simulation Differentiators
Immersive Interprofessional, Multidisciplinary Simulation Education
Unlike traditional simulation centers that may focus on a specific field or discipline, our center creates realistic scenarios that bring together professionals from various fields to collaboratively address complex situations.
This approach not only enhances individual skill proficiency but also fosters teamwork and communication across different specialties.
Utilization of Multiple Simulation Centers for Milestone Competency
Our residency utilizes four simulation centers, each with different technological and innovative capabilities. This allows our simulation faculty to design simulations to meet resident milestones whether they are common or high-acuity, low-occurrence (HALO) scenarios, or standard emergency medicine cases. This includes procedural, patient care, and teamwork/communication competencies. The residency program emphasizes incorporating social determinants of health into patient care throughout the emergency department. Our simulation team collaborates with the Global and Population Health division, Drs. Sonnenberg and Pavlic, to incorporate social and population determinants of health into learning objectives for our simulation sessions to further this training.

