Immunotherapy Breakthroughs in Lymphoma Treatment Show the Power of Translational Research
When it comes to the distance between the bench and bedside, the gap does not get much smaller than with Bryon Johnson, PhD. As professor of medicine and director of the Bone Marrow Transplant & Cell Therapy Lab at the Medical College of Wisconsin (MCW), Dr. Johnson’s participation in clinical research to harness the immune system to fight cancer is showing promising results for patients with lymphoma. But his research also has a deeply personal meaning since Dr. Johnson is himself a survivor of this cancer.
“I experienced knee pain for years. I thought it was from a high school sports injury, but it was becoming more consistently painful,” he recalls. In 1990, one year after coming to MCW as a postdoctoral research fellow, Dr. Johnson went to see a doctor to have it looked at more closely. An MRI and biopsy revealed he had a form of B-cell non-Hodgkin lymphoma in his femur. His prognosis was good, but he needed to undergo six months of chemotherapy and radiation.
“Going through treatment gave me a greater appreciation for the struggles people with these types of cancers endure,” Dr. Johnson says. “I was fortunate that my cancer was curable.”
Although traditional cancer treatments such as chemotherapy and radiation offer patients a prolonged life, their side effects may also cause long-term health issues such as weakened bones, heart and lung problems, nerve damage and more. Ten years after treatment, Dr. Johnson experienced a traumatic injury due to radiation weakening of his femur.
“I was playing tennis, and the femur fractured as I planted my leg,” he relates. “I had a lot of blood flow to the fracture area and significant scar tissue, so as a result I could not bend my knee.”
Dr. Johnson had arthroscopic surgery and now has nearly full use of his knee, but his injury is an example of the kinds of long-term consequences of traditional cancer treatments patients face.
Now, Dr. Johnson is leading the way to develop immunotherapy treatment options that reduce or eliminate these kinds of long-term side effects. He oversees the clinical laboratory portion of MCW’s chimeric antigen receptor (CAR) T-cell therapy program, which combines efforts of researchers and clinicians across MCW, the Froedtert & MCW health network, Children’s Hospital of Wisconsin and the Versiti BloodCenter of Wisconsin to modify patients’ T cells and equip them to work with their own immune system to fight cancer.
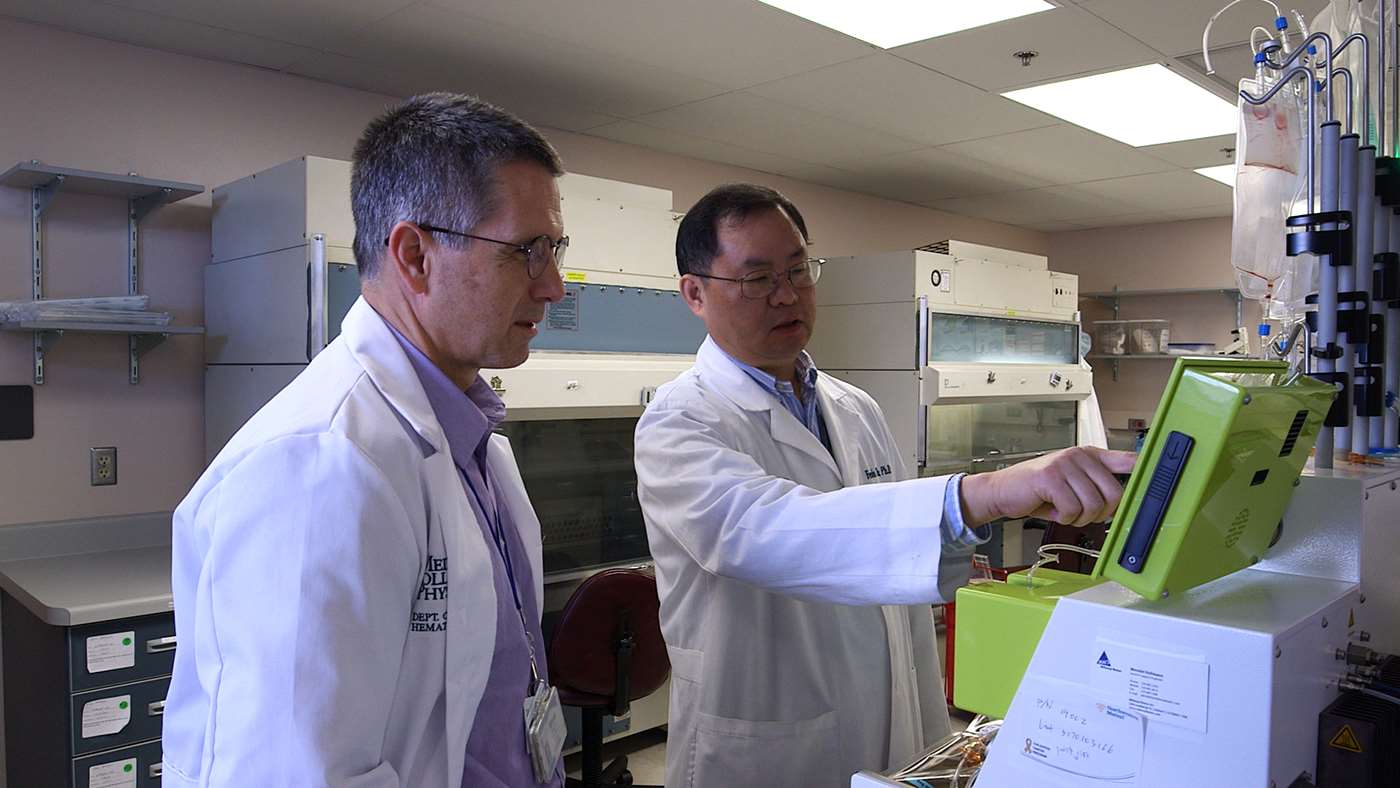
“Our CAR-T cell program is a collaborative effort involving nurses, physicians, coordinators and researchers. Our clinical lab provides one piece of a larger effort,” he says. Dr. Johnson’s team uses a novel, self-contained technology called the CliniMACS Prodigy® device to isolate and modify a patient's own T cells to express new antigen receptors. Since CAR-T cell therapy uses a patient’s own cells, each therapy is tailored for the individual patient. Once the modified T cells, now “energized fighter cells,” are returned to the patient’s blood stream, they target specific proteins located on the cancer cells.
Dr. Johnson works closely with his assistant lab director, Fenlu Zhu, PhD, and his clinical partner, Nirav Shah, MD, MSHP, both assistant professors of medicine in MCW’s division of hematology and oncology, to minimize the amount of time it takes for patients to go from trial enrollment to receiving the CAR-T cell therapy.
“The Food and Drug Administration (FDA) has approved use of this device to create the CAR-T cells in our own lab, so we have a very fast, 14-day turnaround time for patients to receive their modified cells. We are hoping to reduce that time even further to 10 to 12 days,” he says. Another novel aspect about MCW’s CAR-T cell program, Dr. Johnson explains, is they have engineered cells to target two proteins instead of one.
“Cancer cells are good at hiding from the immune system. This presents a challenge for researchers because if a cancer loses the target protein when only one is being targeted, it can no longer be seen by the CAR-T cells,” he says. “But by targeting two proteins, the chances are much better the treatment will still work.”
Dr. Johnson and the entire CAR-T cell therapy team have seen impressive early results, and Dr. Shah recently presented their research at the 2019 American Society of Clinical Oncology (ASCO) meeting in Chicago. In phase I of the clinical trial, patients were given low, medium and high doses of CAR-T cells to test safety, but also observed very promising early efficacy. Now, the team is looking forward to moving into phase II of the trial to test clinical response and efficacy more thoroughly. They are also planning to begin trials using the same treatments in childhood cancer patients later this year.
“This is the most exciting work I have done in my career,” Dr. Johnson says. “Although I am in the lab and not coming face-to-face with patients, there is a very direct connection for me with how this research is making an impact in the clinic. It is truly translational research.”
Although chemotherapy and radiation won’t go away, Dr. Johnson explains, immunotherapy can be used alongside conventional treatments to reduce the intensity of those treatments and corresponding patient side effects. Because of his own experience facing cancer, Dr. Johnson says he understands how difficult the short- and long-term side effects can be for patients and their families.

“I am excited for the potential to use CAR-T cell therapy early to avoid the long-term side effects of traditional chemotherapy,” he says. “Cancer patients often feel sick, and they and their families also have to endure the many ups and downs throughout treatment. Immunotherapy has the potential to be curative for more and more patients. It is not a miracle drug, but as we refine the process over time, we may be able to give patients more options. It will become one of the new ‘arts of medicine’ as physicians learn to combine immunotherapy and other new treatments with hopefully less intensive chemotherapies and radiation to more strategically tailor unique options for each individual patient. It will not be ‘one size fits all.’”
Dr. Johnson predicts CAR-T cell immunotherapy will also soon become a useful form of treatment for solid cancers such as lung, colon and breast.
“Everything in science takes longer than we want, but I predict in the next five to 10 years, we will see some more amazing breakthroughs in cancer immunotherapy. We want to provide more, better treatment options, and we will be able to offer some real, definitive hope. We all want to reach a 100 percent cure rate. For me, that day cannot come soon enough.”
Featured in this story

Bryon D. Johnson, PhD
Professor, Pediatrics (Hematology/Oncology/BMT) and Microbiology & Immunology
Cancer immunology and immunotherapy
Fenlu Zhu, PhD
Assistant Professor




