MCW Researcher Studying Traumatic Brain Injuries Highlights Need for Better Data in Critical Decision Making
Staff at U.S. hospitals often need to make quick decisions – within 48 hours – about whether to take a patient with severe traumatic brain injury off life-sustaining treatment.
 “Often, they're doing that based on their experience, without much data to inform such a critical decision for a given patient,” says Michael McCrea, PhD, ABPP, co-director of the Neurotrauma Research Center and director of the Brain Injury Research Program at the Medical College of Wisconsin (MCW). “These decisions are made when family and friends of the injured patient find themselves in their darkest hour, and they look to the clinical team for guidance.”
“Often, they're doing that based on their experience, without much data to inform such a critical decision for a given patient,” says Michael McCrea, PhD, ABPP, co-director of the Neurotrauma Research Center and director of the Brain Injury Research Program at the Medical College of Wisconsin (MCW). “These decisions are made when family and friends of the injured patient find themselves in their darkest hour, and they look to the clinical team for guidance.”
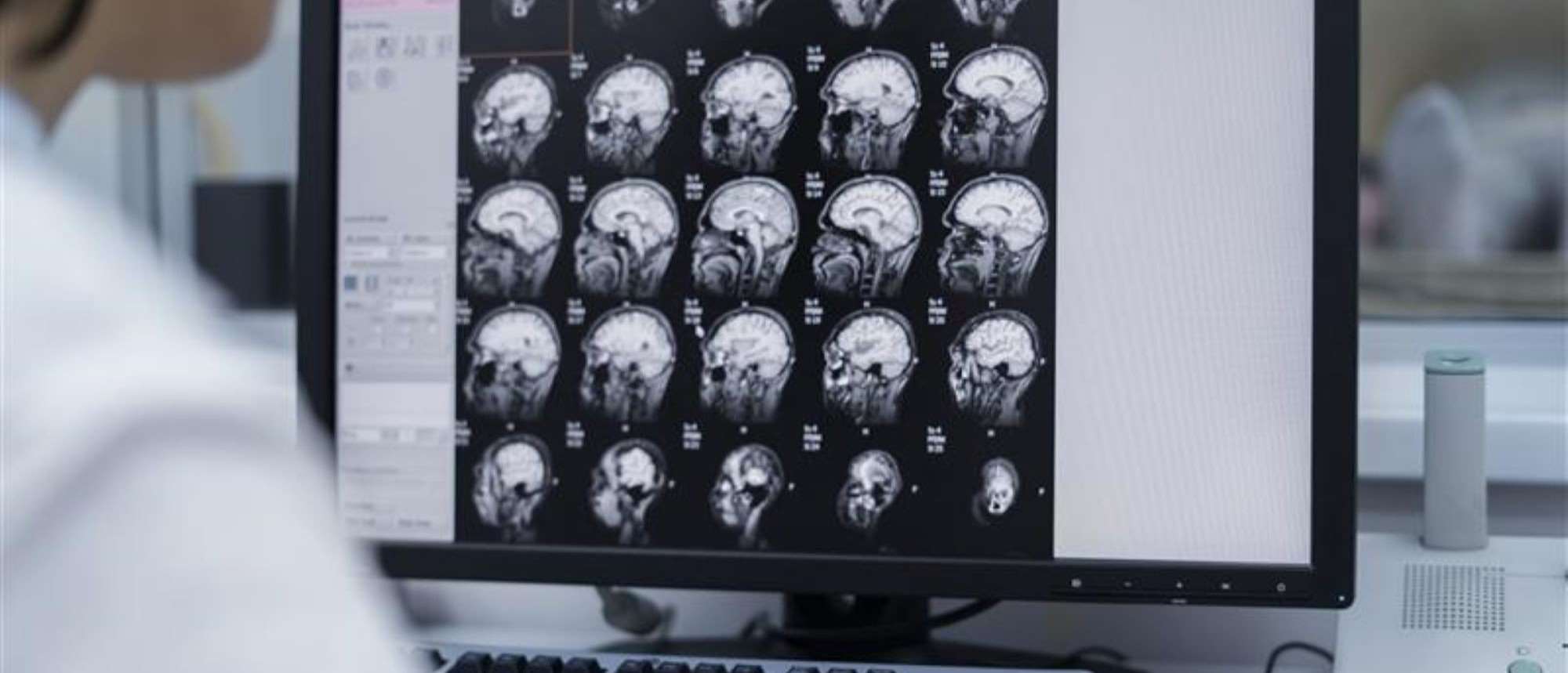
For more than half a century, assessment of acute traumatic brain injuries (TBI) has been done using the Glasgow Coma Scale, which classifies a patient’s injuries as “mild, moderate, or severe” based on their responses to verbal, motor, and other stimuli.
“When I got involved in traumatic brain injury research, we commonly assessed patients by asking blunt questions such as “How many fingers am I holding up?” or “Where are we?” Dr. McCrea says. “Clinicians, researchers, and patients all recognize that we need to do better in our assessment and classification of this complex injury.”
New Methods Advance TBI Treatment
Decades of work by Dr. McCrea, his team, and other brain injury experts have advanced TBI testing to include more measures that can substantially improve treatment and outcomes for patients and prevent premature discussions about whether life support should stop.
“The overarching focus of our work is to improve diagnostic, prognostic, and treatment interventions for patients with traumatic brain injury,” says Dr. McCrea, also the Shekar N. Kurpad, MD, PhD, Chair in Neurosurgery.
For instance, doctors can use blood-based biomarkers to predict the presence or absence of a traumatic hemorrhage and other pathologies. The biomarkers allow specialists to use a blood test to quickly identify who has a brain bleed, which reduces the need for radiation exposure from CT scans by about one-third in patients with an extremely low likelihood of traumatic injury.
“When someone comes in with concerns for hemorrhage or structural brain injury from trauma, such as a motor vehicle crash, we use a CT scan. But a high proportion of CTs come back negative, expending time and cost that could be prevented by the rapid blood tests that are now effective in ruling out brain bleeds,” Dr. McCrea says.
Understanding Populations at High Risk for TBI
According to the CDC, TBI resulted in more than 69,000 deaths in America in 2021. The most common causes are falls, firearm injuries, vehicle crashes, and assaults. Certain groups, including racial and ethnic minorities, service members and veterans, and people who experience homelessness, are at a higher risk of dying or experiencing long-term injuries from TBI.
Dr. McCrea and his team have studied three distinct populations at high risk for TBI: military personnel and veterans, athletes with sports-related concussions, and civilians who come into the level 1 trauma center at Froedtert Hospital and Children’s Wisconsin.
“Work that we have done in one population has translated to those other two populations in almost every instance for the last 30 years,” he says.
The tests they use to examine TBI among the groups have revealed a number of biomarkers that when measured together have not just improved diagnostic accuracy, but can also help predict recovery at two weeks, or three, six, or even 12 months.
Dr. McCrea and other researchers use the biomarkers along with other measures, including a patient’s social environment, to personalize TBI treatment. The group authored a research paper calling on the medical establishment to implement their new framework using those tools along with traditional Glasgow measures as the gold standard in treating TBI.
Dr. McCrea and several members of the MCW faculty recently contributed to the National Institutes of Health-National Institute of Neurological Disorders and Stroke (NINDS) TBI Classification and Nomenclature Initiative, including Lindsay Nelson, PhD, ABPP, Timothy Meier, PhD, and Benjamin Brett, PhD, from the department of neurosurgery and Danny Thomas, MD, MPH, in the department of pediatrics. All were selected based on their national recognition as experts in TBI care and research.
The culmination of this work was published in Lancet Neurology, proposing new standards for the classification and characterization of acute TBI, and featured in a New York Times article. Dr. McCrea was senior author of the article, and Drs. Nelson, Meier, Brett, Thomas and others at MCW contributed greatly to the project.
Partnering with Health Tech Companies, the Department of Defense
Pushing his research beyond the lab and into hospitals has involved forging partnerships with various groups, says Dr. McCrea, including Abbott Laboratories to run biomarker tests on their I-Stat devices or working with the U.S. Department of Defense to conduct research with military personnel.
Dr. McCrea’s team is also currently preparing to participate in a national clinical trial through MCW’s Building Resilience through Action in VEterans and First Responders (BRAVE) program that is going to look at rehabilitative interventions.
MCW has positioned his team to stay at the forefront of research and be among the first that industry and research leaders want to collaborate with, says Dr. McCrea. Part of that is a result of the environment at MCW, which fosters and supports research, innovation, and partnerships.
“We have something very special here at MCW and in the Department of Neurosurgery,” Dr. McCrea says. “We’re very proud of the reputation we’ve built around the country and the globe. That’s a credit to the outstanding work of all our faculty and staff who are dedicated to discoveries that improve the lives of those affected by brain injury.”



