MCW Scientist Focuses on Biomechanical Signaling to Study how to Enhance Lung Regeneration

Akiko Mammoto, MD, PhD, an associate professor in pediatrics at the Medical College of Wisconsin (MCW), began her scientific career as an OB/GYN. In her hometown of Osaka, Japan, she worked as a physician for several years but soon realized she really wanted to be a researcher.
 “I went back to school to get a PhD,” she says. “For a time, I did a lot of basic science research on molecular mechanisms. Then I got the opportunity to come to the U.S. as a postdoc in Donald Ingber’s lab at Harvard Medical School and Boston Children’s Hospital.”
“I went back to school to get a PhD,” she says. “For a time, I did a lot of basic science research on molecular mechanisms. Then I got the opportunity to come to the U.S. as a postdoc in Donald Ingber’s lab at Harvard Medical School and Boston Children’s Hospital.”
There she discovered her life’s work: researching angiogenesis, the body’s process of making new blood vessels from existing ones and, specifically, how that process works in the lungs.
In Ingber’s lab she learned many approaches to manipulate biomechanical properties in the body, including blood flow, tissue stiffness, and stretching forces, which determine how cells grow and differentiate into different types.
With that knowledge, she and her husband Tadanori Mammoto, MD, PhD, also an associate professor in pediatrics at MCW, developed a method to place soft, gel-like material called fibrin directly onto the surface of a living mouse’s lung. The animal’s lung cells then grew into the gel, allowing them to see new blood vessels forming in real time.
“We can change the components and stiffness of the gel and mix different types of cells in the gel to mimic the lung’s micro-environment,” she says.
Increasing the Speed of Angiogenesis in Lungs
Dr. Mammoto and her husband joined the MCW faculty in 2016 and developed their own lab, where they have continued studying the mechanism of angiogenesis.
They explored how angiogenesis leads to lung regeneration in mice by taking out one of the lobes from a mouse lung and analyzing the re-growth of the remaining lobes. They found that when one lung lobe is removed, the expression of several genes and proteins changes and helps trigger blood vessel growth that promotes tissue regeneration.
They have also found that angiogenesis and lung growth are inhibited in older mice, and that obesity inhibits angiogenesis, but that the drug AdipoRon can improve lung regeneration in obese mice.
Dr. Mammoto says genes and proteins that accelerate the speed of angiogenesis and lung regrowth may help patients recover from a plethora of lung diseases such as chronic lung infections – sometimes derived from COVID-19 or flu infection – and diseases like pulmonary fibrosis.
When the lung regrows after part of a lobe is removed, she says, the remaining lung stretches as it expands to fill the empty space in the chest. This mechanical signaling is new and important for angiogenesis and regrowth of the lung.
New Grant to Study Key Protein Paxillin
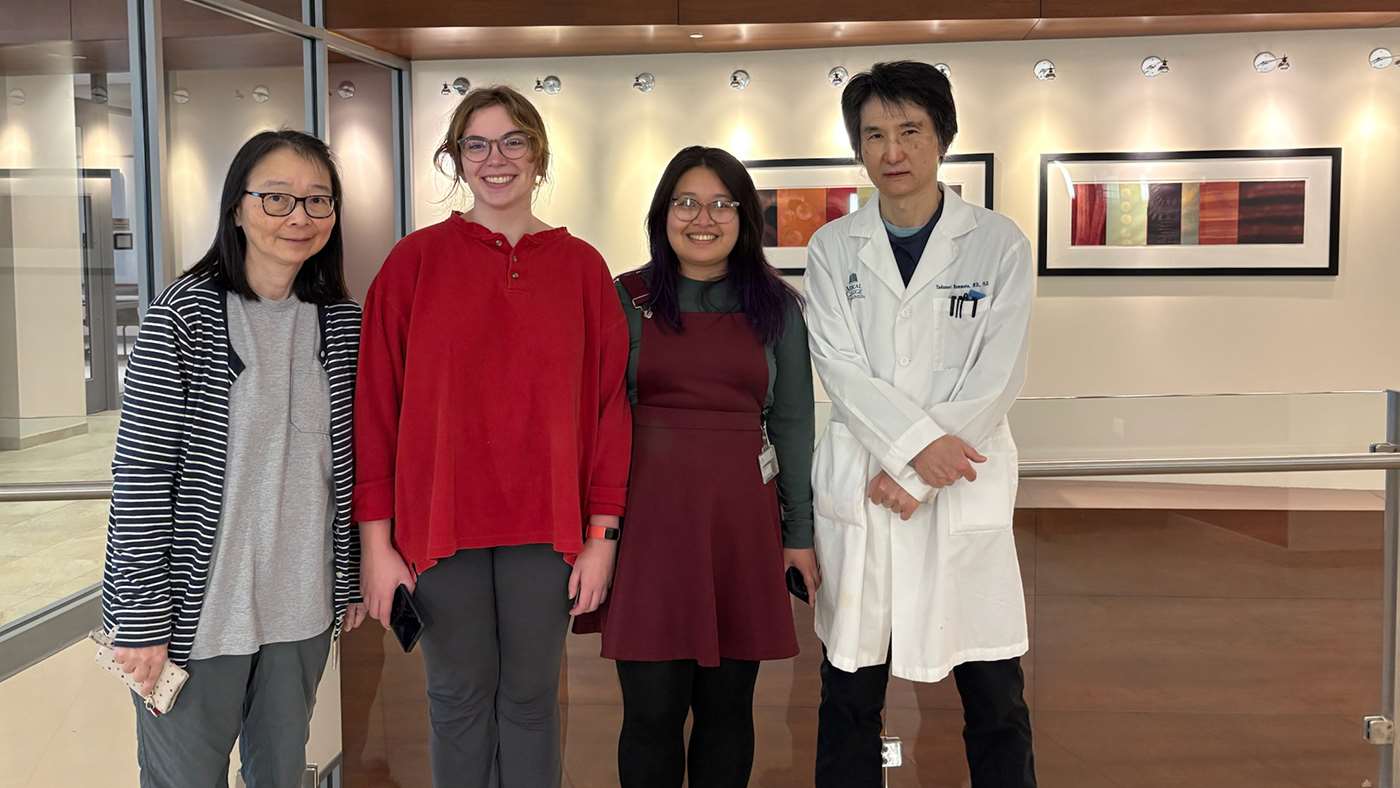
The lab of Dr. Akiko Mammoto (far left) is studying the role that the protein paxillin plays in lung regeneration.
Now Dr. Mammoto has a new $2.4 million R01 grant that will fund more angiogenesis research. Dr. Mammoto will observe the phenomenon of stretching in different locations of the lungs when part of the lung is removed, and how the cells in the lung can sense this stretching and respond by growing new blood vessels that help with lung repair and regeneration.
A protein called paxillin detects those stretching forces, Dr. Mammoto says, and the new grant will help her zero in on paxillin’s potential role as a key protein that helps guide new blood vessel growth after lung removal.
Years ago, she found that when the protein is removed from a cell, angiogenesis stops in the neonatal eye. More recently, her lab also demonstrated that paxillin is important for neonatal lung development.
“Modulating the expression of paxillin could speed up the process of angiogenesis,” she says. “We’re going to try to figure that out.”