Seeing the Unseen: Advanced Ocular Imaging Bridges Research and Patient Care
The Medical College of Wisconsin (MCW) Eye Institute doesn’t just blur the line between research and patient care, it erases it.
This seamless integration is at the heart of the Dennis P. Han, MD Advanced Ocular Imaging Program (AOIP) and the work of its co-director, Joseph J. Carroll, PhD, ’02, a professor in the Departments of Ophthalmology & Visual Sciences, Biophysics, Biomedical Engineering, and Cell Biology, Neurobiology and Anatomy.
Dr. Carroll’s pioneering research in retinal imaging has revolutionized the way we understand and treat retinal diseases, empowering clinicians to provide life-changing care for patients who once had no options.
Mapping the Retina with Adaptive Optics Imaging
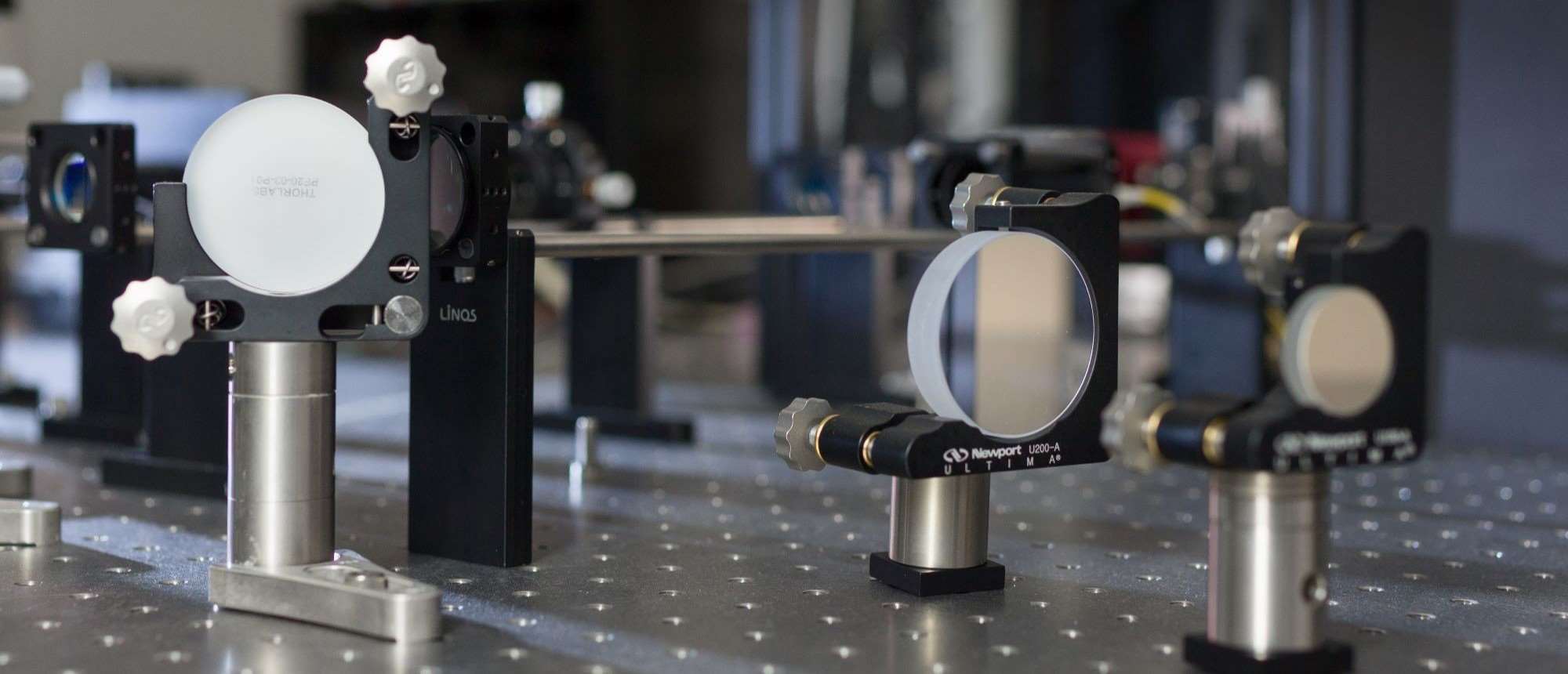
 Dr. Carroll (pictured right) focuses on the relationship between structure and function in the human visual system, both in health and disease. Using advanced imaging tools like adaptive optics and optical coherence tomography, his team can visualize the retina at a cellular level, revealing details that are invisible using conventional clinical equipment.
Dr. Carroll (pictured right) focuses on the relationship between structure and function in the human visual system, both in health and disease. Using advanced imaging tools like adaptive optics and optical coherence tomography, his team can visualize the retina at a cellular level, revealing details that are invisible using conventional clinical equipment.
“The goal is to develop a better understanding of how the retina works and how it fails in disease,” says Dr. Carroll. “By applying high-resolution imaging, we can see things that were previously unseen.”
One of the most groundbreaking technologies developed at AOIP is “split detector” adaptive optics imaging, which enables researchers to map the retina with unprecedented detail, allowing clinicians to visualize individual cells, blood vessels, and subtle abnormalities that might otherwise go undetected.
This level of detail is not just academically fascinating – it’s clinically transformative. For patients with complex retinal conditions, this imaging technology provides a roadmap for treatment, guiding surgeons to areas of the retina that need intervention.
From the Lab to the Operating Room
At the MCW Eye Institute, the AOIP is not just a research lab – it’s a bridge between discovery and treatment.
“Over the years, we’ve built an infrastructure that allows us to see patients in a high-throughput fashion and at a relatively low cost,” says Dr. Carroll. “The physical separation of research and clinic spaces can often be a detriment to work like ours. Here, we’re an elevator ride from each other, and that’s not always the case at other places with similar imaging technology.”
This integration was put to the test in the case of a patient with severe vision distortion caused by an epiretinal membrane – a thin layer of scar tissue that forms on the retina. Traditional clinical imaging couldn’t provide the granularity needed to locate the membrane, leaving the patient without treatment options.
When the patient was brought to the AOIP, Dr. Carroll’s team used split detector adaptive optics imaging to create a detailed map of the retinal surface, which revealed the defect.
“The imaging allowed us to see the membrane clearly,” says Dr. Carroll. “After discussing the images with the patient, they requested that we provide them to Dr. Han, who would be performing the surgery to remove the membrane. He printed a large, high-resolution map of the retina to use as a guide in the operating room. It was a perfect example of how research can directly impact patient care.”
Removing the membrane, which was invisible to the naked eye, required inserting instruments into what appeared to be a normal retina.
 “We had to trust the technology to guide us,” says Dennis Han, MD, (pictured right), retired MCW professor, a renowned vitreoretinal surgeon and one of the founding directors at AOIP.
“We had to trust the technology to guide us,” says Dennis Han, MD, (pictured right), retired MCW professor, a renowned vitreoretinal surgeon and one of the founding directors at AOIP.
With the images as a guide, Dr. Han successfully removed the membrane, relieving the distortion in the patient’s retina.
“The next day, when we took off her patch, the patient knew immediately that she was better,” Dr. Han recalls. “Usually, it takes three to six months for patients to notice improvement, but she saw it right away. She was ecstatic.”
For the patient, the results were life changing. She could remove the traffic cones she had placed around her house to help her navigate around furniture and between rooms and regained the ability to move through her world with confidence.
One of those traffic cones now resides in the AOIP to illustrate for students and staff the potential impact of their work.
“She was so grateful for the improvement in her vision,” says Dr. Han. “It was a reminder of why we do what we do.”
A New Standard of Care
The success of this case underscores the transformative power of translational research. By combining cutting-edge imaging technology with clinical expertise, the AOIP has set a new standard for treating complex retinal conditions.
“The technology itself isn’t unique,” says Dr. Carroll. “It’s the infrastructure, the clinical coordinators, the engineers, and the ability to support patients that make it special. We’re a bona fide translational research unit, and that’s the secret sauce.”
This approach has far-reaching implications. For patients, it means access to treatments that were once unimaginable. For clinicians, it provides tools to make more informed decisions. For researchers, it offers a direct pathway to see their work make an impact on real lives.
Dr. Carroll continues to push the boundaries of retinal imaging, developing new technologies and refining existing ones.
Fifteen years ago, he and Dr. Han envisioned the AOIP as a collaborative hub where researchers, engineers, computer programmers, and optics experts could come together to develop and refine imaging tools. Their goal was to create a space that not only fosters innovation in device development but also ensures that clinicians have access to advanced imaging technologies to improve patient care.
The AOIP is also expanding its reach, collaborating with other institutions and sharing its expertise through training programs.
“The imaging makes a difference in terms of the diagnosis, and our goal is to make this technology and our translational approach available to as many people as possible,” says Dr. Carroll.



