Medical College of Wisconsin Health Psychology Residency Clinical Rotations & Didactics
Adult Track Clinical Rotations
Adult Track Continuity Clinic | Behavioral Medicine and Primary Care (BMPC) Psychology Clinic
Amber Craig, PhD; Larry Miller, PsyD
The Behavioral Medicine and Primary Care (BMPC) Psychology Clinic is a collaborative care clinic focusing on serving patients referred by primary care and medical subspecialty providers without integrated health psychology services in their clinics. The BMPC Clinic is housed in the Department of Psychiatry and Behavioral Medicine and is an outpatient, ambulatory clinic.
Patients referred to the BMPC clinic have a variety of presenting problems including adjustment, to physical health conditions and/or treatments, primary or comorbid mental health concerns (e.g., depression, anxiety, trauma), or engaging in healthier habits (e.g., improved sleep, increasing physical activity, smoking cessation). Psychology residents will perform empirically informed health psychological assessments and brief interventions to promote symptom reduction, self-management of mental and physical health conditions, function status, and quality of life, which include but are not limited to: Problem Solving Therapy, Cognitive Behavioral Therapy, Mindfulness Based Stress Reduction, and Acceptance and Commitment Therapy.
Direct Services
The goals of this clinic include optimizing patient health and quality of life through the assessment and management of their symptoms, barriers, and functional status.
- Assessment – clinical biopsychosocial interviews and health psychology assessments.
- Health & Behavior Intervention – healthy diet, exercise, sleep, reduction of substance misuse, stress management, behavioral pain management, medication adherence, and health-related communication skills.
- Brief Psychotherapy– anxiety, depression, health-related traumatic responses, substance use, adjustment to life changes, and management of personality disorders in patients who are medically complicated.
- Group treatment – co-facilitation of a 6 week “ACT for Chronic Illness” group, as well as opportunities for the creation of treatment groups.
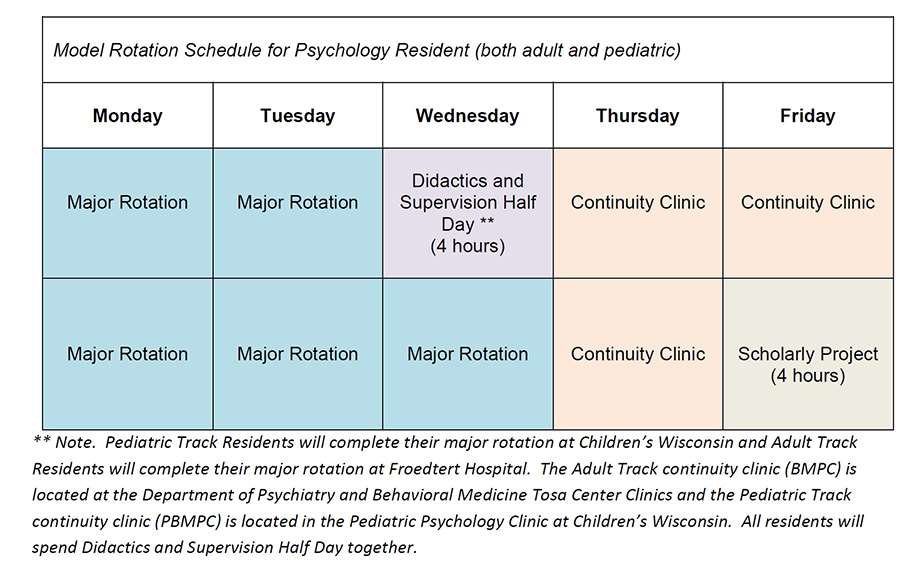
Following the Four Quadrant Clinical Integration Model, psychology residents will maintain a psychologically and medically diverse BMPC outpatient caseload throughout the entire training year. Psychology residents will also have the opportunity to carry some cases on a long-term basis where the presenting concern is managing chronic illness. Residents will also have the opportunity to learn how to manage an outpatient caseload throughout the training year, in providing courses of care to a diverse set of patients. The BMPC clinic operates on Thursdays and Fridays.
Integrated Behavioral Health
Since the COVID-19 pandemic, in concert with other health settings and systems, referred patients have presented with greater health complexities. Psychology residents will work to understand the reasons for referral to the clinic, and evaluate patients’ needs to devise a plan of care that fits within the scope of the clinic. They will collaborate with multiple health professionals through the electronic medical record system, phone consultation, and collaborative practice; and refer patients to the other needed services and provide bridge care as appropriate. Psychology residents will become familiar with coordinating care across multiple treating providers in multiple locations. Activities include:- Co-treat with other disciplines to more effectively address mental or behavioral health concerns and communicate via medical record and other forms of technology.
- Consult with staff regarding patients’ psychological functioning via electronic medical record.
- Be available for behavioral health consultation from providers in the health enterprise as requested.
- Consult on behavioral management interventions via medical record and/or phone to help medical providers effectively manage challenging behaviors while providing care.
Pediatric Track Clinical Rotations
Pediatric Track Continuity Clinic | Pediatric Behavioral Medicine and Primary Care (PBMPC) Clinic
Jacqueline Kawa, PhD; Jacquelyn Smith, PhD
The Pediatric Behavioral Medicine and Primary Care Psychology (PBMPC) clinic is a collaborative care clinic focusing on serving patients referred by primary care pediatrics and pediatric subspecialty providers without integrated health psychology services in their hospital-based clinics. The PBMPC Clinic is housed in the Department of Pediatrics section of Pediatric Psychology and Developmental Medicine at Children’s Wisconsin and is an outpatient, ambulatory clinic.
Patients referred to the PBMPC clinic have a variety of presenting problems including adjustment to physical health conditions and/or treatments, mental health concerns (e.g., depression, anxiety), behavioral concerns (e.g., impulse control problems, oppositional behaviors), learning concerns and/or academic performance concerns (e.g., attention problems, learning disability), or failure to engage in healthier habits (e.g., adherence to medical regimen, increasing physical activity). Psychology residents will perform empirically informed assessments and brief interventions. In addition to their weekly supervision of therapy cases, residents will receive bi-weekly supervision from a testing faculty member on a minimum of eight assessment cases per year. Residents will independently conduct evaluation intakes and provide families with feedback on assessment results.
Testing Faculty Members: Margaret Altschaefl, PhD, Adiona Mustafaraj, PsyD
Direct Services
The goals of this clinic include optimizing patient health and quality of life through the assessment and management of their symptoms, barriers, coping, and functional status.
- Assessment – Tests of intellectual, academic, and executive functioning; parent, teacher, and self-report rating scales; personality inventories; clinical biopsychosocial interviews; and health psychology assessments. Each resident will conduct monthly assessment batteries (intake assessment, testing, and feedback) under the supervision of a primary testing supervisor competing a minimum of 8 full batteries over the year.
- Health & Behavior Interventions – healthy lifestyle promotion, sleep training, procedural anxiety management, coping with chronic health conditions, pain management, and medication adherence
- Brief Psychotherapy – anxiety, depression, health-related traumatic responses, ADHD, and adjustment to life changes. Therapeutic interventions utilized include but are not limited to Parent-Child Interaction Therapy (PCIT), Parent Management Training (PMT), Cognitive behavioral therapy (CBT), Behavioral therapy (BT), Motivational Interviewing (MI) and Acceptance and Commitment Therapy (ACT), Unified Protocol (UP).
Integrated Behavioral Health
Psychology residents will collaborate with multiple health professionals through the electronic medical record system, phone consultation, care conferences, and other collaborative practice. Psychology residents will become familiar with coordinating care across multiple treating providers in multiple locations. Activities include:
- Multidisciplinary and interdisciplinary treatment to more effectively address mental or behavioral health concerns and communicate via medical record and other forms of technology
- Consult with staff regarding patients’ psychological functioning via electronic medical record
- Be available for behavioral health consultation from providers in the health enterprise as requested
- Consult on behavioral management interventions via medical record and/or phone to help medical providers effectively manage challenging behaviors while providing care to patients