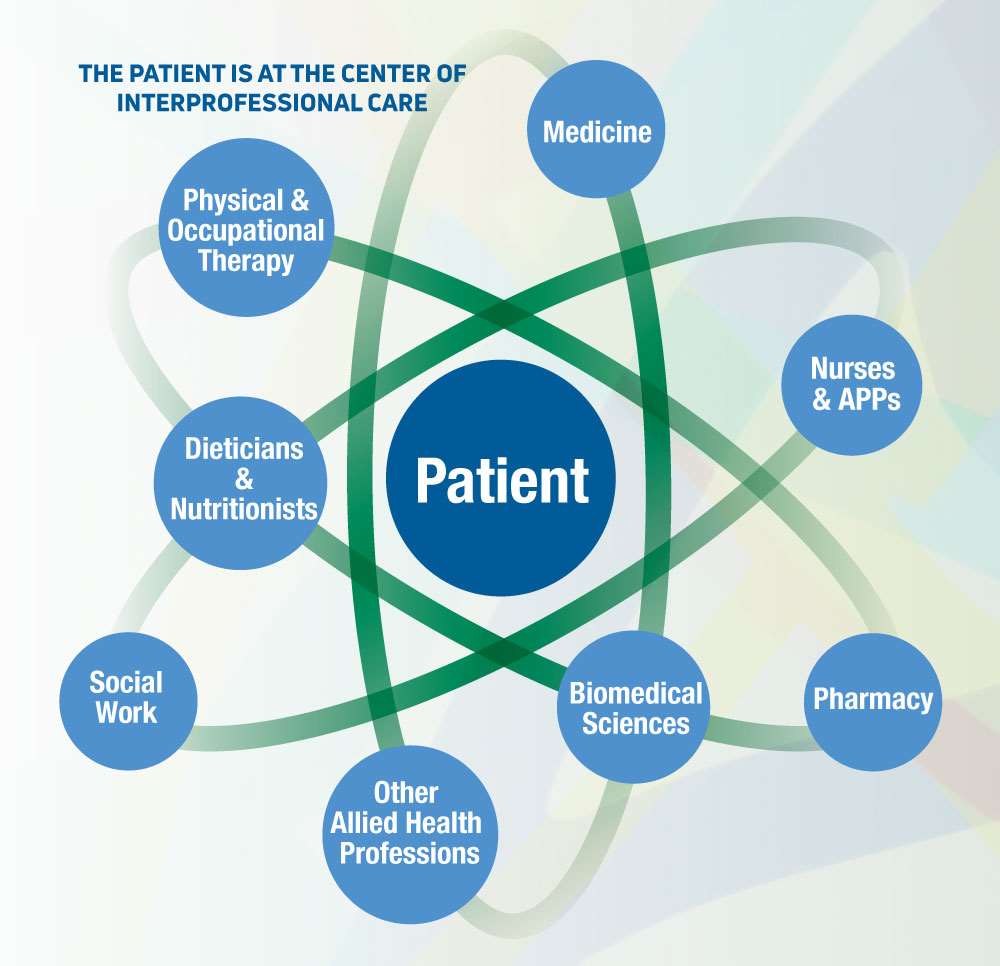
The Importance of Interprofessionalism: Clinical Care

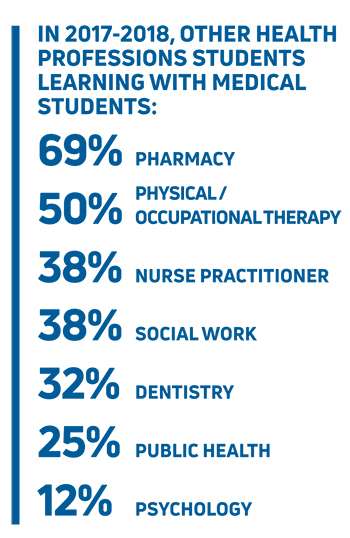
The Summer 2019 issue of MCW Magazine features a cover story on interprofessionalism and how it influences learning, care and collaboration among students, healthcare providers and scientists. This second installment in a two-part series focuses on interprofessionalism in clinical care. (Source for all infographics: Association of American Medical Colleges.)
Cellular Therapies for Patients with Blood Cancers and Hereditary Blood Disorders
The Froedtert & the Medical College of Wisconsin health network (Froedtert & MCW) offers experimental and FDA-approved cellular treatments for cancerous and noncancerous conditions.
“We use cells to treat human disease,” says Parameswaran Hari, MD, FEL ’02, MS ’06, MCW professor of medicine and chief of the division of hematology and oncology. “The main modality is blood and bone marrow transplant – which means that we use bone marrow stem cells, blood stem cells, cord blood cells, immune cells and genetically modified cells to treat patients. Whenever you use cells to treat human disease, the cellular therapy program is involved.” Healthcare professionals at Froedtert & MCW treat about 300 cellular therapy patients per year – or about six per week.
Dozens of individuals are involved in interprofessional patient care in the cellular therapies program at Froedtert & MCW. “While any specialty can be involved, there are several core groups. The ‘transplanters’ themselves are oncologists, hematologists or hematologist/ oncologists,” according to Dr. Hari.
“The most important interprofessional groups are our nurses and our advanced practice providers (physician assistants and nurse practitioners). The nurses are highly trained, highly professional cell therapy nurses who provide day-to-day care of the patients and who know exactly what to look out for in terms of complications. The cell therapy specialists act as the quarterbacks – but we wouldn’t be able to survive without the team. Specialized nurses who work as blood and marrow transplant (BMT) coordinators follow each patient along, from the time he/she makes the first visit through treatment and all the way to discharge.”
In addition to the core interprofessional teams, there are numerous other specialists, including the cell processing laboratory (comprising basic scientists and cell therapy technicians); cell collection specialists (the apheresis teams); pharmacists who have advanced training in cellular therapies; immunologists; pathologists; and intensivists. “Our hospital has one of the best hematopathology teams I’ve ever worked with, and our ICU team is especially geared toward taking care of critically ill patients,” Dr. Hari shares.
A third group within the interprofessional team comprises endocrinologists, infectious disease specialists, physical therapists and rehabilitation services, social workers, discharge specialists, schedulers, medical assistants, dieticians and nutritionists. Other medical specialists are added as needed. “The best thing about Froedtert & MCW is that our team members are all very cheerful and collegial. They love what they’re doing and are very focused on the patients. This is a unique team with many moving parts, yet it still works well. The most effective team is one that is glued together, having worked together for many years,” Dr. Hari adds.
According to Dr. Hari, the benefits to the patients from such a critical interprofessional team is that there is more brain power invested in their care than in a place where no such team exists. “Everyone becomes highly skilled and specialized in their respective areas, and they know how to work well with each other. It’s all about the depth and breadth of care – and all of medicine is increasingly becoming team-based like this,” he says.
The care providers also benefit from working in an interprofessional environment – as it reduces medical error and enhances support by adding layers of safety, decreases anxiety levels and improves team spirit and outcomes.
Students benefit as well. “This is where and how they should learn,” notes Dr. Hari. “They get to see the breadth of care that can be delivered at a high level. They can learn teamwork in medicine, which is very difficult to achieve right away without actually training for it. Students can learn not just medicine, but how care should be harmoniously coordinated.”
The program is under the overall leadership of the program director, currently Mehdi Hamadani, MD, who is responsible for direction, quality and clinical vision.
The doctor in charge of each hospitalized patient meets with her/his team daily to discuss that patient. Once a week, all of the extended teams meet to discuss current patients, upcoming patients and recently discharged patients. Additionally, a quality manager tracks outcomes, infections and every other measure of quality, and maintains/reviews the quality dashboard. Froedtert & MCW’s blood and marrow transplantation program has a better-than-expected survival rate as reported by the Stem Cell Transplant Outcomes Database, and is one of the few programs in the country to achieve this for the past five years, according to Dr. Hari. “Fewer than 10 percent of the BMT programs in the US beat the expected survival odds for their patients – and we are one of those programs year after year.”
Interprofessionalism is a critical component of the best practices in patient care. “In the end, it’s all about communication and the degree to which each team member is willing to respect each person’s expertise,” says Dr. Hari. “Everyone respects everyone else’s roles, regardless of the job title. You respect them for their skill, commitment and role on the team – and there is a considerable amount of consensus-building.”
Hip Fracture Program
The incidence of hip fractures in the US among adults ages 65 and older is staggering. More than 300,000 individuals are hospitalized each year for hip fractures – 95 percent of which result from falling. And approximately 30 percent of seniors fall each year, according to United Health Foundation’s America’s Health Rankings.
The risk of hip fracture increases significantly with age due to decreased bone density and muscle mass. Women are especially at risk, experiencing three-quarters of all hip fractures due to bone density loss following menopause.
Within Froedtert & MCW, an average of 30-40 patients per month ages 65+ are treated in the Emergency Department (ED) for hip fractures. But thanks to an innovative new hip fracture program, outcomes for these patients are increasingly more positive.
According to Joseph M. Schwab, MD ’06, GME ’11, MCW assistant professor of orthopaedic surgery and director of the Froedtert & MCW hip fracture program, “About four to five years ago, we started looking at creating a coordinated pathway for patients who arrived at the ED with hip fractures that would take them from presentation at the ED to discharge (and sometimes post-discharge) by providing them with multidisciplinary care provided by interprofessional teams and supported by evidence-based medicine.”
“The goal was to reduce all of the bad stuff that can happen to people who have hip fractures,” he continues. “Most of our patients are elderly, and they can end up with problems like delirium, lengthy hospital stays and variability of care – so we wanted to ensure that we were addressing those patients as quickly as possible without duplicating efforts. By creating an interprofessional team with a pathway, we all know what the rules are and how we manage each step.”
Once the hip fracture has been confirmed, the ED staff activates the hip fracture protocol. A single page goes out to every appropriate team member. The most critical team members include the orthopaedist, who looks at the films and determines the surgical plan; the perioperative medicine specialist, who performs the intake on the patient; the anesthesiologist, who evaluates available time and space in the operating room; and a regional pain specialist, who performs a nerve block to keep the patient comfortable until surgery while minimizing opioids. In addition, nutritionists help provide guidelines for patients’ nourishment and hydration before surgery (which is important in treating the elderly).
Post-surgery, interprofessional team members include the floor nursing staff, physical therapists, pharmacists and social workers who determine patients’ post-acute care.
These patients also interact with a fragility fracture liaison, according to Dr. Schwab. Because almost all hip fractures are fragility fractures – which is a harbinger of osteoporosis – advanced practice registered nurses who work on the surgical floor provide education on osteoporosis and arrange for patients to be seen in the Bone Health Clinic as part of their follow-up care. About 70 percent of Froedtert & MCW’s hip fracture patients follow up at the Bone Health Clinic.
Froedtert & MCW’s hip fracture program, which launched in early 2017, enables patients to be treated more quickly, in a more coordinated fashion and with an interprofessional team. Prior to launch, the average wait time for a patient to have surgery was about 38 hours; with this new protocol, patients are going into surgery in less than 24 hours. “This is significant because patients over 65 who come into the ED with a hip fracture have a shockingly high mortality rate in the first year. That rate is much higher the longer that surgery is delayed,” Dr. Schwab shares.
Dr. Schwab notes that the care providers benefit because “the better you can do for a patient, the better everyone feels. You also gain trust in your fellow teams. When you create an interprofessional team, and you have everybody relinquishing control to the bigger group and following the same protocol, you actually gain trust in one another.”
He adds that the unintended consequence of this is educational. “We have such a close interdisciplinary relationship with our team members that now our residents rotate on some of their services, where they didn’t previously. For example, our ortho interns now rotate on the perioperative medicine service. And observing the interprofessional team model is what medical students see when they rotate with us.”
An interprofessional performance improvement team meets monthly to assess data from the hip fracture program.
Not only patients are taking notice of the new hip fracture program. Recently, Dr. Schwab received a phone call from the chair of orthopaedic surgery at Yale Medical School who wants to establish a consortium of six to eight such programs around the country – including MCW’s – that would structure a national program based on best practices.
SpineCare
The four outpatient SpineCare Clinics within the Froedtert & MCW health network use an interprofessional and transdisciplinary approach to diagnosing and treating neck and back pain that emphasizes early intervention and comprehensive, evidence-based spine care.
SpineCare is a program of the department of neurosurgery and is led by Shekar N. Kurpad, MD, FEL ’01, PhD, Sanford J. Larson, MD, PhD, Chair and Professor of Neurosurgery; and Marjorie Wang, MD, FEL ’06, MPH, professor and vice chair of clinical operations. The team includes neurological and orthopaedic fellowship-trained spine surgeons, physical medicine and rehabilitation specialists, neurologists, chiropractors, pain psychologists, spine-trained nurse practitioners and physician assistants. Angela Jolivette, APNP, MSN, leads SpineCare’s team of advanced practice providers.
 The team also includes physical and occupational therapists who focus on spine rehabilitation – such as ergonomics, spine health and exercises that develop core muscle groups to support the spine. “The goal is for patients to make a lifestyle change that incorporates exercise into their daily routine and provides them with the education and tools to enable them to take care of themselves so they don’t have to constantly come back for tweaking and more treatments,” says Mary Jo Widmann, RN, BSN, program manager for MCW’s department of neurosurgery and SpineCare.
The team also includes physical and occupational therapists who focus on spine rehabilitation – such as ergonomics, spine health and exercises that develop core muscle groups to support the spine. “The goal is for patients to make a lifestyle change that incorporates exercise into their daily routine and provides them with the education and tools to enable them to take care of themselves so they don’t have to constantly come back for tweaking and more treatments,” says Mary Jo Widmann, RN, BSN, program manager for MCW’s department of neurosurgery and SpineCare.
“Our doctors like to see patients when they are in the acute to sub-acute stage – somewhere in the 12-week range of when the injury occurred. We like to get people in, get to the source of their problem, treat that problem, and then get some great outcomes for them by giving them the right tools,” she continues.
SpineCare patients – of whom about 40 percent are self-referred – are almost always seen at one of four Milwaukee-area clinics within ten days of calling for an appointment. The clinics average about 700-900 new patients per month – which isn’t surprising given that back pain is the third most common reason for visits to the doctor’s office, according to the American Chiropractic Association. As many as 90 percent of individuals report at least one episode of back pain during their working lives, and back pain is a major cause of disability. In 2018 alone, about 7,330 new patients were treated at SpineCare.
The benefit to the patient of being cared for by an interprofessional team is a seamless experience, Widmann notes. “We can easily see patients within a short window of time because the advance practice providers can do a full workup and order further tests if needed. Sometimes we get patients in to see the chiropractor first. The chiropractor can then make recommendations about where the patient should go next, so the patient doesn’t have to delay treatment. A good percentage of patients who see the advanced practice provider don’t have a surgical pathology. We tell them, ‘Let’s get you going in the right direction without having to wait to see a surgeon.’ This expedites diagnosis and treatment,” she continues.
Widmann adds, “We offer a comprehensive care package the minute patients walk in the door. It’s one-stop shopping. It’s the convenience factor. All our records are in one place. All the providers know one another and can do a curbside consult. We have a terrific robust team that individualizes care to benefit the patient.”
The care providers benefit too. “It’s easy for them,” Widmann explains. “Everything is right there. Everyone knows what their role is. The environment is a pleasant one. There is tremendous respect for one another as colleagues. It’s truly a well-oiled machine, firing on all cylinders.”
The interprofessional environment is meaningful to students as well, according to Widmann. “For the last two semesters, we’ve had chiropractor interns. They are amazed and have never seen anything like what we do at SpineCare. The neurology and PM&R residents who rotate through SpineCare really enjoy it; they love the interaction and the collaborative feel – and they see how the patients are benefitting.”
Widmann continues, “In addition, providers have come in for interviews from other institutions and are impressed about how the interprofessionalism makes a huge difference in patient care. There are few truly integrated programs like ours around the country. Our interprofessional team works seamlessly to get the patient on the right track as quickly as possible.”
Little wonder that 95 percent of SpineCare patients recommend the program to others.



