The Importance of Interprofessionalism: Education and Research

The Summer 2019 issue of MCW Magazine features a cover story on interprofessionalism and how it influences learning, care and collaboration among students, healthcare providers and scientists. This first installment in a two-part series focuses on interprofessionalism in education and research. (Source for all infographics: Association of American Medical Colleges.)
Our ever-changing healthcare system is marked by the increasingly complex health needs of patients – and requires innovative and efficient models of patient care. These models, in turn, require key competencies – such as effective communication, teamwork and interprofessional collaboration among healthcare professionals. An effective interprofessional collaboration helps ensure high-quality patient care and is having a positive impact on team members who work together daily.
Individuals with differing perspectives in healthcare offer unique ideas and talents to help improve patient care. By promoting a constant exchange of expertise, interprofessionalism helps to break down barriers among everyone involved in patient care – resulting in better learning and the best possible health outcomes. In both clinical practice and education, interprofessionalism encourages a focus on teamwork – based not on a specialty or hierarchy, but rather on effectiveness and outcomes.
In today’s healthcare workplaces, interprofessional patient care isn’t the exception – it’s the new norm. Whether practicing in a hospital, clinic or primary care office, medical professionals work side by side with a multitude of other healthcare disciplines, including nurses at different levels, certified medical assistants, dietitians, nutritionists, pharmacists, physician assistants, social workers, mental health workers, health navigators, health coaches, community health workers, exercise physiologists and quality improvement and informatics specialists. This means that students must be prepared to work on multidisciplinary teams from day one.
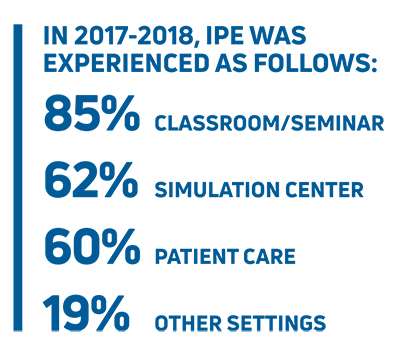
 To that end, an important component of interprofessionalism is interprofessional education (IPE) – a model in which individuals from two or more professions in healthcare learn together during all or part of their professional and postgraduate training with the goal of cultivating collaborative practice. This form of education is particularly effective in subspecialties, in which the need for interprofessional collaboration and learning is most acute. IPE helps develop and promote interprofessional thinking and acting; promotes beneficial information and knowledge exchange and mutual understanding; and ensures the acquisition of shared knowledge.
To that end, an important component of interprofessionalism is interprofessional education (IPE) – a model in which individuals from two or more professions in healthcare learn together during all or part of their professional and postgraduate training with the goal of cultivating collaborative practice. This form of education is particularly effective in subspecialties, in which the need for interprofessional collaboration and learning is most acute. IPE helps develop and promote interprofessional thinking and acting; promotes beneficial information and knowledge exchange and mutual understanding; and ensures the acquisition of shared knowledge.
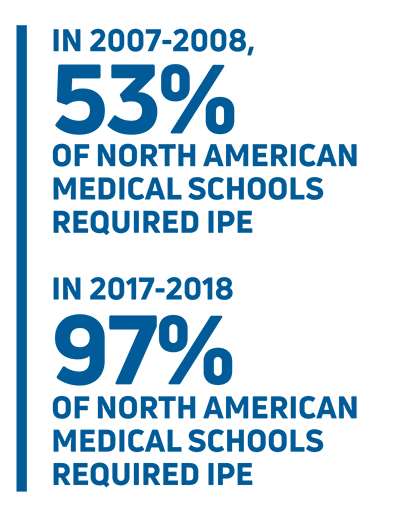
In 2007, the Association of American Medical Colleges (AAMC) released its strategic priorities, clearly stating that IPE and interprofessional practice were key areas of focus. Shortly thereafter, many medical schools began to actively incorporate some form of IPE into their curricula to prepare students for a future of healthcare in a patient-centered, team-oriented system. IPE focuses on values and ethics; roles and responsibilities; interprofessional communication; and teams and teamwork.
Several advantages of IPE have been reported, including increased mutual respect and trust; improved understanding of professional roles and responsibilities; effective communication; increased job satisfaction; and positive impact on patient outcomes. Studies have shown that students trained in an IPE approach have better interprofessional collaborative practice competencies compared to students without IPE training. This can be attributed to students’ more positive attitudes toward each other, a better understanding about each other’s competencies, the ability to share knowledge and skills and improved team identity.
MCW has embraced interprofessionalism and IPE across its missions of education, clinical care, research and community engagement – positioning team-based patient care and team-based learning as hallmarks of its successful approach to 21st-century healthcare.
What follows is a glimpse into MCW’s commitment to interprofessionalism and IPE through the lens of students, healthcare providers and scientists – although this merely scratches the surface of the institution’s interprofessional endeavors.
Interprofessional Education
MCW School of Medicine
The MCW School of Medicine’s Milwaukee campus offers IPE sessions for many of its 11 early clinical and basic science courses as well as some elective Pathway courses. IPE sessions offered in 2018-2019 included collaborations with nursing, physical therapy, clinical and medical laboratory science students, dietetic interns from area institutes of higher learning and MCW School of Pharmacy students. The sessions included simulations, interactive activities and case-based discussions focused around the health needs of the patient. “The IPE sessions offer a realistic view of the work experience and allow students to practice using the communication and collaboration skills they need to optimize team-based care,” says Erica Y. Chou, MD ’09, pediatric hospitalist, director of medical school interprofessional education, and curriculum pillar faculty member for MCW’s Robert D. and Patricia E. Kern Institute for the Transformation of Medical Education (the Kern Institute).
Third-year medical student Monique Graf participated in six IPE sessions during her first two years, helping organize several. “Each of the professionals approaches the patient and case from a different perspective,” Graf says. “We are trained differently, but we all have the same goal of doing what’s best for the patient – and that requires we come together when developing a care plan.”
David Holzer, also a third-year medical student, says the IPE sessions helped him learn his course materials more effectively. “During our hematology unit, the lab tech students who worked with us did an excellent job teaching me how to analyze a blood smear. We learned from their unique strengths and wisdom, just as we shared ours with them.”
MCW-Green Bay and MCW-Central Wisconsin have comparable IPE sessions for their students, but also offer unique sessions that take advantage of their respective regional partnerships. For example, James R. Warpinski, MD, course director of the continuous professional development course in the second year at MCW-Green Bay, coordinates a session that brings together medical students and social work students to diagnose and treat geriatric patients. As part of the session, teams observe and discuss works of art – an exercise that improves their ability to function as a team and teaches them to respect each other’s opinions.
The Kern Institute
The Kern Institute, launched in 2017, employs a variety of methods to enhance medical education. In April 2019, leaders conducted a Design Thinking Workshop that was attended by 180 first- through third-year medical students, and first- and second-year School of Pharmacy students. The course introduced students to the five steps of design thinking, which focus on empathy and the needs of the patient. Instructors walked the students through the process of what a “critically ill patient” experiences, and then they participated in a team-based interdisciplinary exercise in which they used this new creative problem-solving method to design a process improvement.
“Participants learned how to ask effective questions, be excellent listeners and draw informed conclusions,” notes M. Christopher Decker, MD, GME ’98, MCW professor of emergency medicine and director of the culture and systems pillar and the entrepreneurial mindset/design thinking program with the Kern Institute. “The exercise allowed the students to creatively collaborate to find solutions that will benefit the patient.”
Another effort of the Kern Institute is its annual Transformational Ideas Initiative. This year, more than 50 ideas were submitted by faculty, staff and students, and 10 projects were selected to receive funding as well as yearlong technical and coaching support.
MCW School of Pharmacy
The School of Pharmacy’s curriculum was designed to improve how pharmacists contribute to healthcare through interprofessional, team-based practice experiences. Students in the School of Pharmacy’s inaugural class, which matriculated in the summer of 2017, are now entering their Advanced Pharmacy Practice Experience rotations. Students in the doctor of pharmacy (PharmD) program undertake approximately 200 hours of IPE within their lecture- based, clinical and elective courses.
“The MCW School of Pharmacy has integrated IPE into its curriculum from orientation to graduation in order to prepare the next generation of pharmacists to advance healthcare team collaboration and quality of patient care,” says George E. MacKinnon III, PhD, MS, RPh, founding dean of the MCW School of Pharmacy.
Students attend an average of 15 different IPE sessions in classes such as Human Anatomy and Physiology, Principles of Drug Action and Pharmacogenomics, Renal and Cardiovascular, and Patient Care Lab. The School of Pharmacy collaborates with MCW’s doctor of medicine and anesthesiologist assistant programs and has IPE affiliation agreements with five other local academic institutions: Columbia College of Nursing; Marquette University; Milwaukee Area Technical College; Milwaukee School of Engineering School of Nursing; and the University of Wisconsin-Milwaukee. Additional partnerships that could enhance the IPE program are continually being identified.
During IPE sessions, pharmacy students learn about, with and from students from different healthcare professions, including physicians, anesthesiology assistants, nurses, medical interpreters, occupational therapists and physician assistants. The sessions offer a wide range of experiences, from hands-on activities, role-play, lectures, group and case-based discussions to simulations using high-fidelity mannequins and standardized patients.
One notable IPE experience for second-year pharmacy student McKenzie Yerks involved the MCW anesthesiologist assistant (AA) students. “We used mannequin patients that presented with a kind of toxicity syndrome,” he says. Along with his fellow pharmacy students, Yerks worked collaboratively with the AA students to decide how to treat the illness. “It was really neat to see what they were learning in their program and how it applied to what we were learning. The IPE sessions make you more well-rounded.”
Scholarly Pathway courses are multi-year courses with interprofessional components that are undertaken by both medical and pharmacy students and led collaboratively by pharmacy and physician clinicians. These students have four interprofessional Pathways available to them.
Third-year pharmacy student Becka Anton recently finished her coursework in her Bioethics Scholarly Pathway. In class, a student usually presents on a topic, after which group discussions among the medical and pharmacy students ensue. The Pathway course also covers topics that aren’t covered in Anton’s pharmacy classes. “It has exposed me to a lot of difficult situations and opened my mind to think about them in many different perspectives,” remarks Anton.
Nastassjia deBourbon is an MCW medical student in the Health Systems Management and Policy Pathway alongside pharmacy students. “I’m thankful that MCW has these interprofessional sessions. We work together and learn together to form a genuine connection,” she notes.
In addition to Pathway electives, pharmacy students can take part in hands-on IPE exposures at Milwaukee-area sites where they experience interprofessional healthcare teams in action, including the Bread of Healing Clinic and the Saturday Clinic for the Uninsured.
 MCW is one of the few schools in the country that requires all School of Pharmacy students to complete one 10-week IPE introductory clinical rotation in their second year that is precepted by a non-pharmacist. Student Claire Solofra rotated with the hospice and palliative medicine team at Froedtert Hospital and experienced an interdisciplinary team comprising diverse professions such as physicians, nurse practitioners, chaplains and child services. She had the unique opportunity to shadow a chaplain as he interacted with patients. “Sometimes while obtaining medical histories, people mention their religions. Now I am better prepared to respond in that situation.”
MCW is one of the few schools in the country that requires all School of Pharmacy students to complete one 10-week IPE introductory clinical rotation in their second year that is precepted by a non-pharmacist. Student Claire Solofra rotated with the hospice and palliative medicine team at Froedtert Hospital and experienced an interdisciplinary team comprising diverse professions such as physicians, nurse practitioners, chaplains and child services. She had the unique opportunity to shadow a chaplain as he interacted with patients. “Sometimes while obtaining medical histories, people mention their religions. Now I am better prepared to respond in that situation.”
During her rotation, Solofra was consulted by other members of the interprofessional team for questions regarding medications – as there wasn’t a pharmacist located on-site. “Compared to other rotations, this one felt like the most realistic in-practice setting,” she adds.
Interprofessionalism in Science
Research Centers are a Nexus
At MCW, research centers provide an environment in which experts across specialties and departments connect to advance team science. Some research centers focus on scientific fields such as population health while others are more narrowly focused on biological systems or specific diseases. The MCW Cancer Center (MCWCC) is an example of a large research center, comprising more than 300 physician and scientist members from more than 40 departments, divisions or institutes at three institutions: MCW; Versiti’s Blood Research Institute; and the University of Wisconsin-Milwaukee.
“The MCW Cancer Center is very active in its efforts to bring clinicians and scientists together across many disciplines,” says Carol Williams, PhD, Joan K. Van Deuren Professor in Breast Cancer Research, professor of pharmacology and toxicology at MCW and co-director of the MCWCC’s Cancer Biology program.
In addition to three overarching research programs – Cancer Biology, Cancer Prevention and Outcomes, and Discovery and Developmental Therapeutics – the MCWCC facilitates interdisciplinary research working groups and disease-oriented research teams that meet regularly to collaborate. Dr. Williams credits these groups and interactions for sparking many new collaborative projects – including two of her own. She works with Jennifer Knight, MD ’04, MCW assistant professor of psychiatry and behavioral medicine, to study how stress may affect certain hormones that, in turn, may promote cancer progression and metastasis.
In addition, Dr. Williams met Mark McNally, PhD, MCW associate professor of microbiology and immunology, at an MCWCC symposium, and together they are now testing prospective cancer therapies. “Mark and I now have a patent on a potential drug with Ionis Pharmaceuticals, and we are working on a manuscript together,” notes Dr. Williams. She doesn’t believe these productive partnerships would have formed without the MCWCC serving as a nexus and helping her to meet, learn from and work with colleagues across MCW.
Clinical and Translational Science
In addition to MCW’s many research centers, the Clinical and Translational Science Institute of Southeast Wisconsin (CTSI) is a major interprofessional hub at MCW – bringing together basic scientists and healthcare providers across MCW and partner academic institutions in the region.
Alison Kriegel, PhD ’08, MCW associate professor of physiology, knows that partnering with physicians to expand on her basic science background helped sharpen the direction of her experiments.
“There are a million questions that I’d love to explore,” she states. “But there simply isn’t enough time. Working with physicians who understand limitations in current treatments and the challenges faced by their patients helps me address clinically impactful gaps in knowledge.”
Dr. Kriegel accelerated her learning curve in clinical and translational science by participating in the Clinical Research Scholars Program, a two-year guided apprenticeship sponsored at MCW by the CTSI. Dr. Kriegel says that this training, along with networking opportunities hosted by MCW’s CTSI, help bring together the worlds of clinical practice and basic science.
“No one can be an expert in everything, so it is really important for physicians and basic scientists to work together,” she says.
Graduate Degree Programs
MCW’s Graduate School partners with the CTSI to offer Master of Science (MS) and Doctor of Philosophy degrees along with a certificate program in clinical and translational science.
“Many master of science degree students are clinicians at early stages of their academic careers. They are interested in forming new collaborations and participating in clinical and translational studies to advance knowledge alongside their treatment of patients,” says Dr. Kriegel.
The MS degree program is designed for healthcare professionals, clinical investigators, research scientists and individuals working in biomedical industries. The certificate program often attracts doctoral students in other Graduate School programs, and the doctoral program caters to students pursuing academic research careers in basic, clinical and translational science.



