Foundation Gift Brings Hope for New Treatments for Multiple Myeloma

The Paula and Rodger Riney Foundation funds scientific research leading to a better understanding and possible cure of multiple myeloma and related cancers. The Rineys are shown above.
A philanthropic investment from the Paula and Rodger Riney Foundation is supporting five related multiple myeloma research projects at MCW that are focused on immunotherapies and investigating long-term survivorship among patients.
“We are pleased to partner with the Medical College of Wisconsin Cancer Center in our shared aspiration of finding a cure for multiple myeloma,” says Rodger Riney. “Since the establishment of the foundation, we have sought out the most innovative work in the field, and we are very excited about the promise MCW’s research shows for treating this complex disease.”
For more than two decades, MCW has worked closely with research and healthcare partners to provide patients with research-based myeloma clinical care and access to some of the most pivotal cancer clinical trials and medical discoveries in the country. This includes critical findings in immune therapies – an approach that deploys the body’s natural immune defenses to slow the spread of cancer cells.
Multiple myeloma is a rare and currently uncurable cancer of the plasma cells, which are white blood cells that make antibodies to fight infections. These abnormal plasma cells build up in the bone marrow and form tumors in many bones of the body. The disease can permanently damage organs and weaken bones, and is two to three times more common in Blacks/African Americans.
MCW was among the first institutions in the world to produce its own source of CAR T cells, a highly promising immunotherapy designed to target two antigens on cancer tumors and provoke an immune response from the body. This work began in 2017 at MCW and its adult healthcare partner, Froedtert Hospital, as part of a phase I clinical trial that resulted in safe and promising outcomes for patients with cancers of the immune system. It is now part of a multi-institution phase II trial to determine outcomes in a larger set of patients.
That work, along with other research, helped to spur the contribution by the Paula and Rodger Riney Foundation, whose contributions are typically directed to an elite group of academic research centers, including the Dana-Farber Cancer Institute, Mass General Cancer Center and the Mayo Clinic.
“We are grateful for this transformative support from the Paula and Rodger Riney Foundation,” says Gustavo Leone, PhD, director of the MCW Cancer Center and the Dr. Glenn R. and Nancy A. Linnerson Endowed Chair for Cancer Research. “There has never been a more exciting time to be at the forefront of this pioneering research. The scientific advancements we will make with this gift will yield much-needed benefits for generations of patients and families facing a diagnosis of multiple myeloma.”
The five projects operating with support from the Riney Foundation enhance MCW’s existing work with immunotherapies and efforts to treat patients who are long-term survivors of myeloma. The projects range from investigations of new therapeutic targets for CAR T cells to work aimed at understanding how patients respond differently to similar therapies.
The promise that immunotherapies (including treatments through CAR T-cell therapies) have for myeloma and other cancers continues to generate enthusiasm from researchers and private and public investments in the field, particularly as evidence started to emerge regarding its effectiveness.
Anthony E. Zamora, PhD, MCW assistant professor of medicine (hematology/oncology) and microbiology & immunology, recalls the widespread excitement that accompanied new discoveries in immunology when he was working on his PhD.
“My decision to pursue cancer research as a career was solidified during my graduate school years studying immunology at UC Davis,” he shares.
“When Science magazine announced in its December 2013 issue that cancer immunotherapy had been named the ‘Breakthrough of the Year,’ it opened the floodgates for those of us exploring ways to modulate the immune system to fight cancer,” he continues.
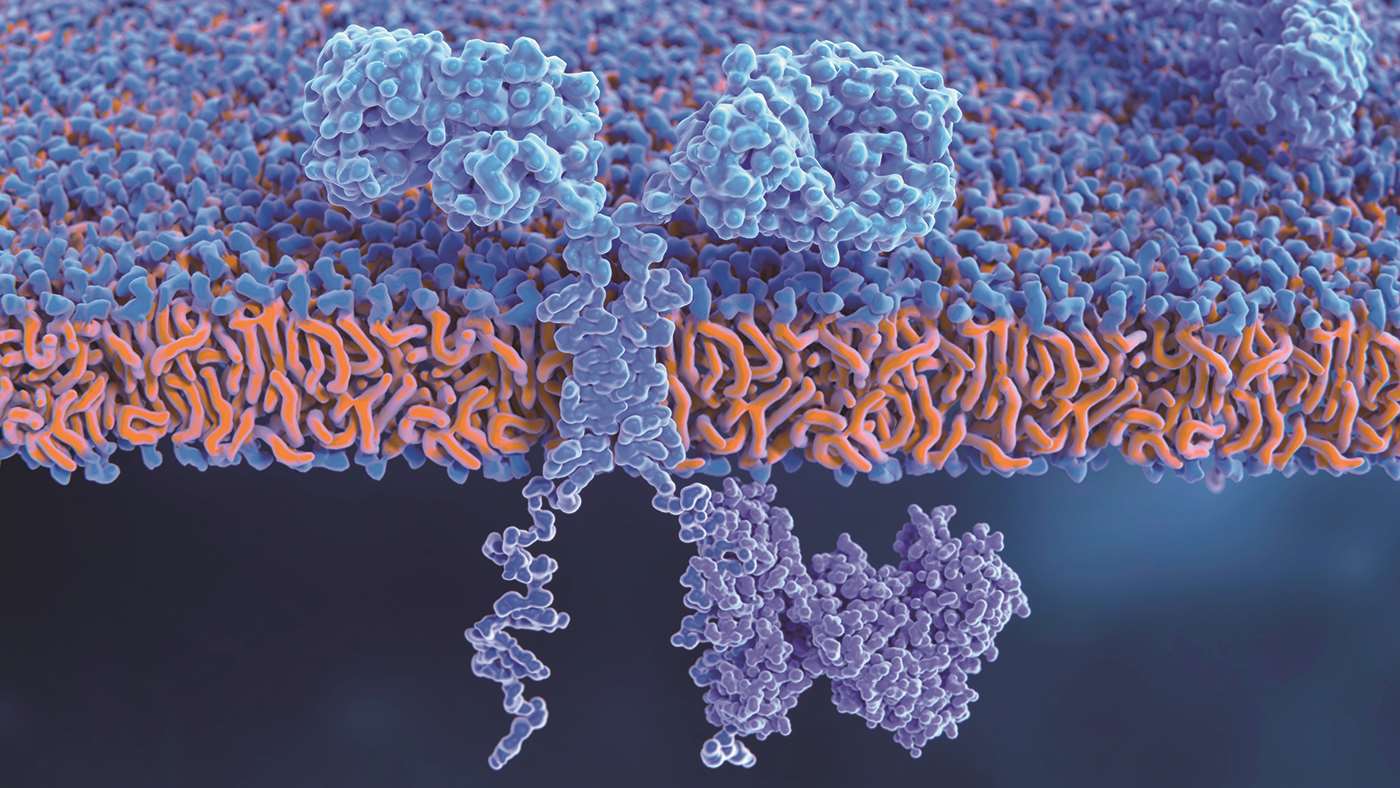
In CAR T-cell therapy, T cells are genetically modified to contain CAR receptors on the cell surface (such as the one depicted at right), which improve their ability to eliminate cancer cells.
Dr. Zamora shares, “The sense of purpose behind the work I was doing was further ingrained into my psyche the first day I set foot on St. Jude Children’s Research Hospital campus as a postdoctoral fellow and saw firsthand how bench-to-bedside research was making an immediate impact on improving survival in children battling this disease.”
“The Riney Foundation gift for these projects is supporting our vision and giving us the opportunity to dream big and continue working toward our goal of eradicating cancer,” Dr. Zamora adds.
– Michael J. Mathias
A Calling of Hope for Rev. Dr. Trinette V. McCray
For many patients undergoing treatments for multiple myeloma, the critical importance of research inspires their own advocacy for expanding scientific discovery.
For Rev. Dr. Trinette V. McCray, informing the community about the importance of supporting cancer clinical trials was a natural extension of her lifelong calling to help others.
 A Milwaukee native who grew up attending Milwaukee Public Schools, Dr. McCray was called to enter the ministry in 1979. A lifelong member of Milwaukee’s faith community, she earned a master’s degree from Morehouse School of Religion and a doctor of ministry degree from Northern Baptist Theological Seminary. She worked at Cardinal Stritch University for 23 years, where she served as a campus minister and the executive director of the Center for Calling and Engagement before her retirement.
A Milwaukee native who grew up attending Milwaukee Public Schools, Dr. McCray was called to enter the ministry in 1979. A lifelong member of Milwaukee’s faith community, she earned a master’s degree from Morehouse School of Religion and a doctor of ministry degree from Northern Baptist Theological Seminary. She worked at Cardinal Stritch University for 23 years, where she served as a campus minister and the executive director of the Center for Calling and Engagement before her retirement.
Three years later, Dr. McCray’s unexpected multiple myeloma diagnosis led to a new calling and a new community to serve.
“I had extreme bone pain and fractures,” she shares.
“My mother had rheumatoid arthritis, so I assumed I had the same. When I went to the doctor for a checkup, the physician assistant suggested that we do an X-ray of the nodules on my lungs – and the results came back suspicious, likely that it was cancer. I had an appointment with a doctor the next morning, who asked if I had ever heard of multiple myeloma,” she notes.
“I had never heard of multiple myeloma,” she admits. “When a person gets a diagnosis of cancer, there is probably no greater sense of vulnerability that comes into one’s heart. I was given two to five years survival.” Since starting treatment, Dr. McCray has been a patient of Anita D’Souza, MD, MS ’15, MCW associate professor of medicine (hematology/oncology).
“I learned that Dr. D’Souza had received her training at the Mayo Clinic and specialized in multiple myeloma,” Dr. McCray adds.
“From our first consultation, Dr. D’Souza put me at ease regarding where I was and what our plan of care options were, which was encouraging. She shared that there are new treatments being developed through clinical trials and getting approved every year. I exhaled,” Dr. McCray continues.
Dr. McCray further says, “I prayed for doctors who would be wise and do what I needed. In working with Dr. D’Souza, she explained to me the benefits of clinical trials. They offer the advantage of the latest medical attempts at securing a cure or remission. I believe that being a part of the trials and the latest treatments helped me surpass my initial prognosis. I’m moving into my ninth year.”
Outside the hospital, Dr. McCray’s calling encourages her to share her experiences with others. “I never knew about multiple myeloma or how it affects the Black community,” she says.
“Black women, especially those over 60, are most affected. My experiences with clinical trials and treatments have helped me bond with relatives of friends and family who are going through this. I also recently connected with the Black Myeloma Health Community through the HealthTree Foundation. I have joined its ‘Spread the Word campaign’ to get the word out to the Black community about multiple myeloma,” Dr. McCray remarks.
“Gifts support research, medical approaches and compassionate care to do whatever is humanly possible. Donors become a part of that human possibility. Together, we can do great things to help bring cures and treatments and extend lives,” Dr. McCray adds.
– Rebecca Schultz



