Collaborative for Healthcare Harm, Hazard, and Risk Reduction and Prevention (CHiRP)

Mission
Core Principles:
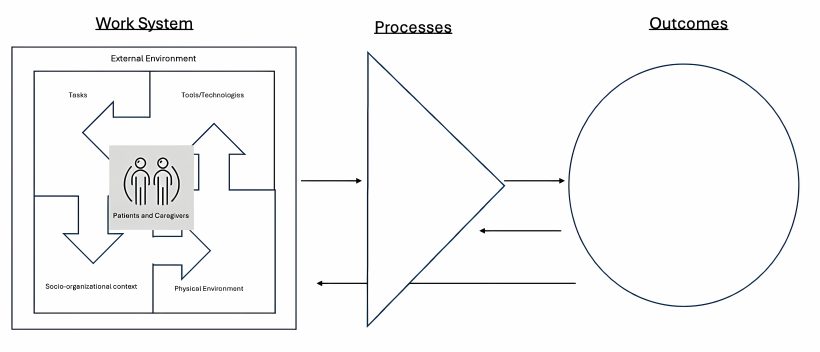
- Healthcare harm is the result of hazards within complex sociotechnical systems- involving people, environments, tools and technology-and their interactions with other system components.
- Healthcare providers are a source of safety through their adaptative actions.
- The phenomena labeled as “error” is a product of complex system interactions and NOT the cause of harm events. Instead, error is a symptom of poorly designed systems
- Harm reduction and prevention require collaboration with non-healthcare disciplines including (but not limited to) human factors engineers, psychologists, experts in design, patients and families, and clinicians.
- That said, zero harm can be an aspiration but never a goal. It is literally impossible to achieve zero harm because the system is complex and dynamic.
Who Should Join?
How to Join
Publications
- Ladell, M. M., Jacobson, N. L., Yale, S. C., McDermott, K. L., Papautsky, E. L., Catchpole, K. R., & Scanlon, M. C. (2025). The problem with how we view medical (and diagnostic) error in emergency medicine. Academic Emergency Medicine, 32(3), 340–347. https://doi.org/10.1111/acem.15076
- Scanlon, M.C., Venkitachalam, R. & Catchpole, K. When is a central venous access device not a central venous access device? When it is a hazard. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03428-5
- Ladell, M. M., Yale, S., Bordini, B. J., Scanlon, M. C., Jacobson, N., & Papautsky, E. L. (2024). Why a sociotechnical framework is necessary to address diagnostic error. BMJ Quality & Safety.
- Snooks KC, Wehrenberg K, Rajzer-Wakeham K, Nelson H, Rothschild C, Rajapreyar P, Luetje M, Scanlon MC, Petersen TL, Meyer MT. (2025) Pediatric Mass Casualty Incident and a Critical Care Response. Disaster Medicine and Public Health. 10.1017/dmp.2025.25
- Schnell JL, Tager JB, Kenney AE, Lim P, Everhart S, Joaningsmei S, Balisteri KA, Morgan-Tautges A, Berridge K, Brophey M, Rothschild C, Scanlon MC, Davies WH, Lee KJ. (2025) Impact of Systems of Care on Emotional Well-Being of Primary Family Caregivers of Children with Medical Complexity. Maternal and Child Health Journal. 10.1007/s10995-025-04066-x
- Scanlon M, Jacobson N. Safety I, Safety II, and the New Views of Safety. PSNet [internet]. Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2025.

