Medical College of Wisconsin Critical Care Medicine Fellowship
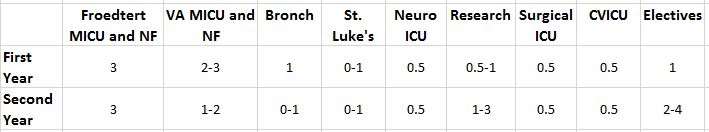
The Critical Care Medicine Program at the Medical College of Wisconsin is a two-year program designed to achieve competence in the basic and clinical aspects of critical care medicine.
Welcome from the Program Director, Rahul Nanchal, MD

About the Fellowship
Frequently Asked Questions
Meet Our Fellows
First Year

Tejaswini Addanki, DO
Critical Care Medicine Fellow
Medical School: Idaho College of Osteopathic Medicine; Residency: Franciscan Health Olympia Fields
Gerardo Rubio, MD
Critical Care Medicine Fellow
Medical School: University of Illinois College of Medicine, Rockford; Residency: Mercyhealth GME Consortium

Sulaiman Sultan, MD
Critical Care Medicine Fellow
Medical School: Ayub Medical College, Abbottabad, Pakistan; Residency: University of New Mexico, Albuquerque, NM

Sara Tesfatsion, MD
Critical Care Medicine Fellow
Medical School: Meharry Medical School; Residency: Medical College of Wisconsin
Second Year

Swati Jain, MD
Critical Care Medicine Fellow
Medical School: Grant Medical College, Mumbai, India; Residency: AtlantiCare, New Jersey, NJ

Anuj Malik, MD
Critical Care Medicine Fellow
Medical School: ACPM Medical College, Dhule, India; Residency: Abington Memorial Hospital, Philadelphia, PA

Jay Patel, MD
Critical Care Medicine Fellow
Medical School: Yale School of Medicine, New Haven, CT; Residency: Vanderbilt University Medical Center, Nashville, TN

Racine Reinoso, MD
Critical Care Medicine Fellow
Medical School: University of Santo Tomas Faculty of Medicine and Surgery, Philippines; Residency: New York Medical College - Metropolitan, New York, NY
Contact Us
Pulmonary and Critical Care Fellowship
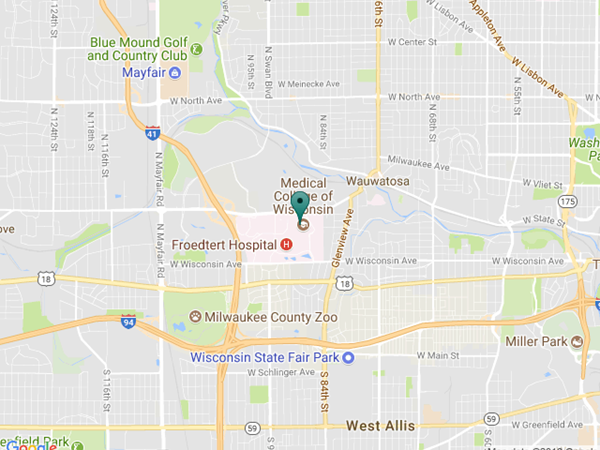
Medical College of Wisconsin
Hub for Collaborative Medicine, 8th Floor
8701 Watertown Plank Rd.
Milwaukee, WI 53226
Fellowship Coordinator
Gabby Zeinert
(414) 955-0437
(414) 955-0093 (fax)
gzeinert@mcw.edu
Program Director
Rahul Nanchal, MD
Professor of Medicine
Division of Pulmonary, Critical Care & Sleep Medicine
rnanchal@mcw.edu
Associate Program Director
Amit Taneja, MD
Associate Professor of Medicine
Division of Pulmonary, Critical Care & Sleep Medicine
ataneja@mcw.edu