Medical College of Wisconsin Pulmonary and Critical Care Fellowship Program
The Pulmonary and Critical Care Fellowship Program at the Medical College of Wisconsin is a combined three-year program designed to provide opportunities to learn the basic and clinical aspects of each of these areas of medicine.
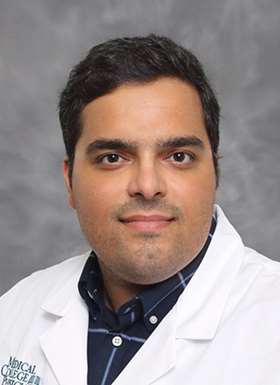
Welcome from the Program Director, Rose Franco, MD
As a former trainee at MCW and now Faculty in our division, I am so proud to work for this institution with such diverse trainees. Every day I learn something new from them. I know that I and our faculty are laying the foundations of great future careers in Pulmonary and Critical Care for all our trainees.
As you review our web pages I hope that you appreciate the depth and breadth of the experience in Pulmonary and Critical Care that we offer for our trainees. As you can also appreciate, many of our former fellows have stayed on as faculty at MCW, a testament to the collegial atmosphere that MCW provides for all!

About the Fellowship
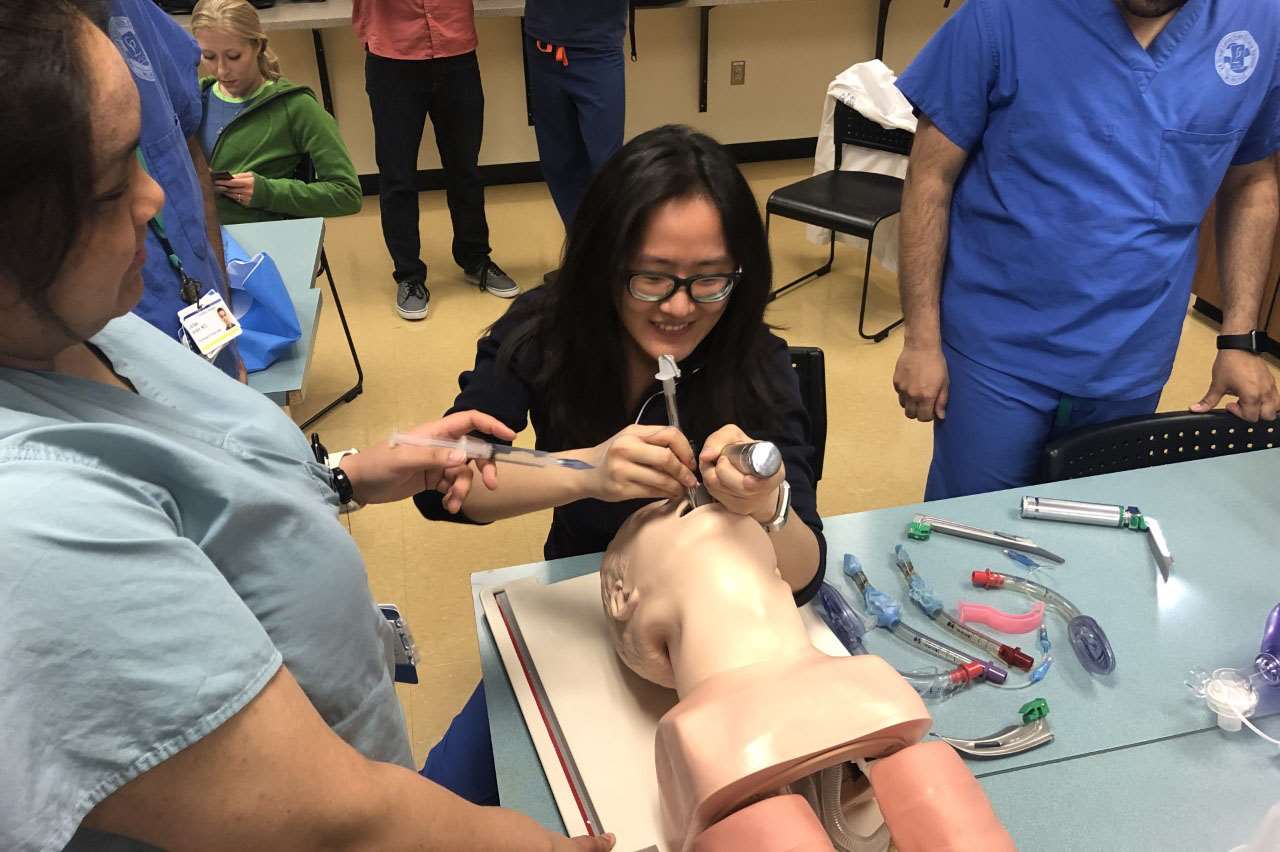
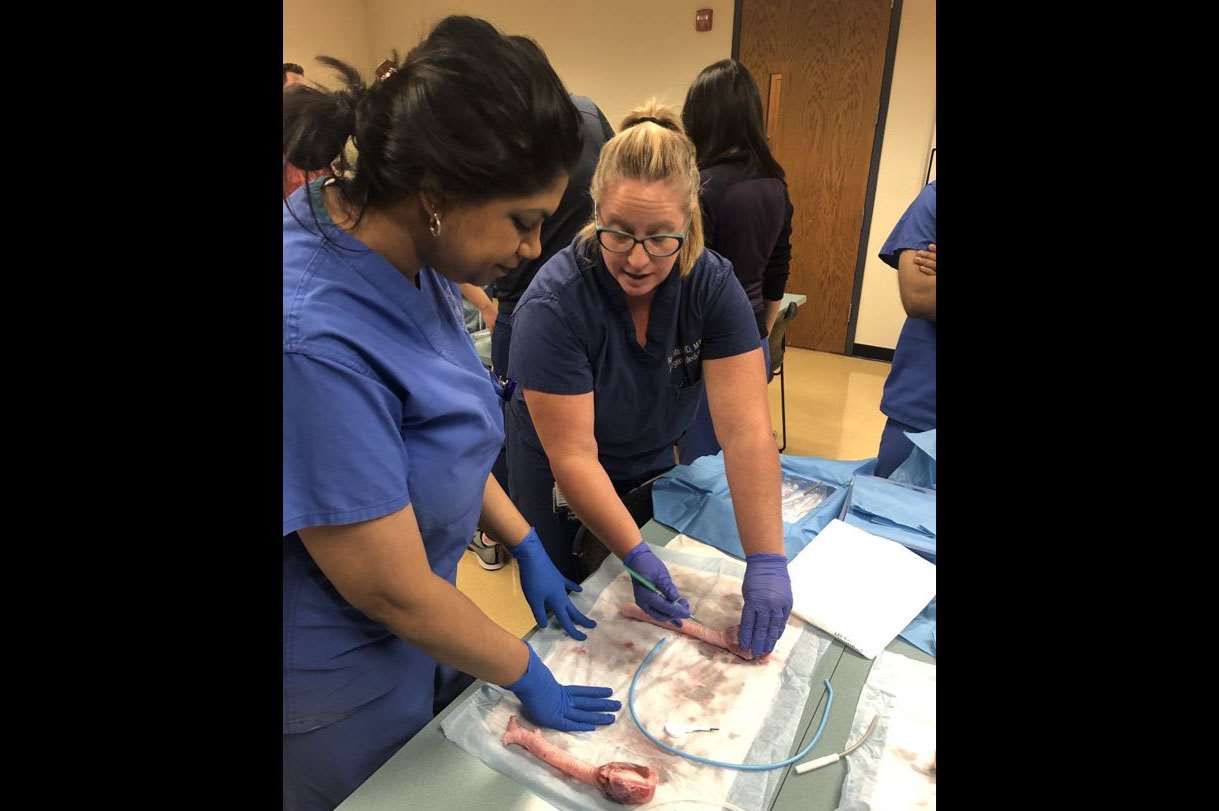
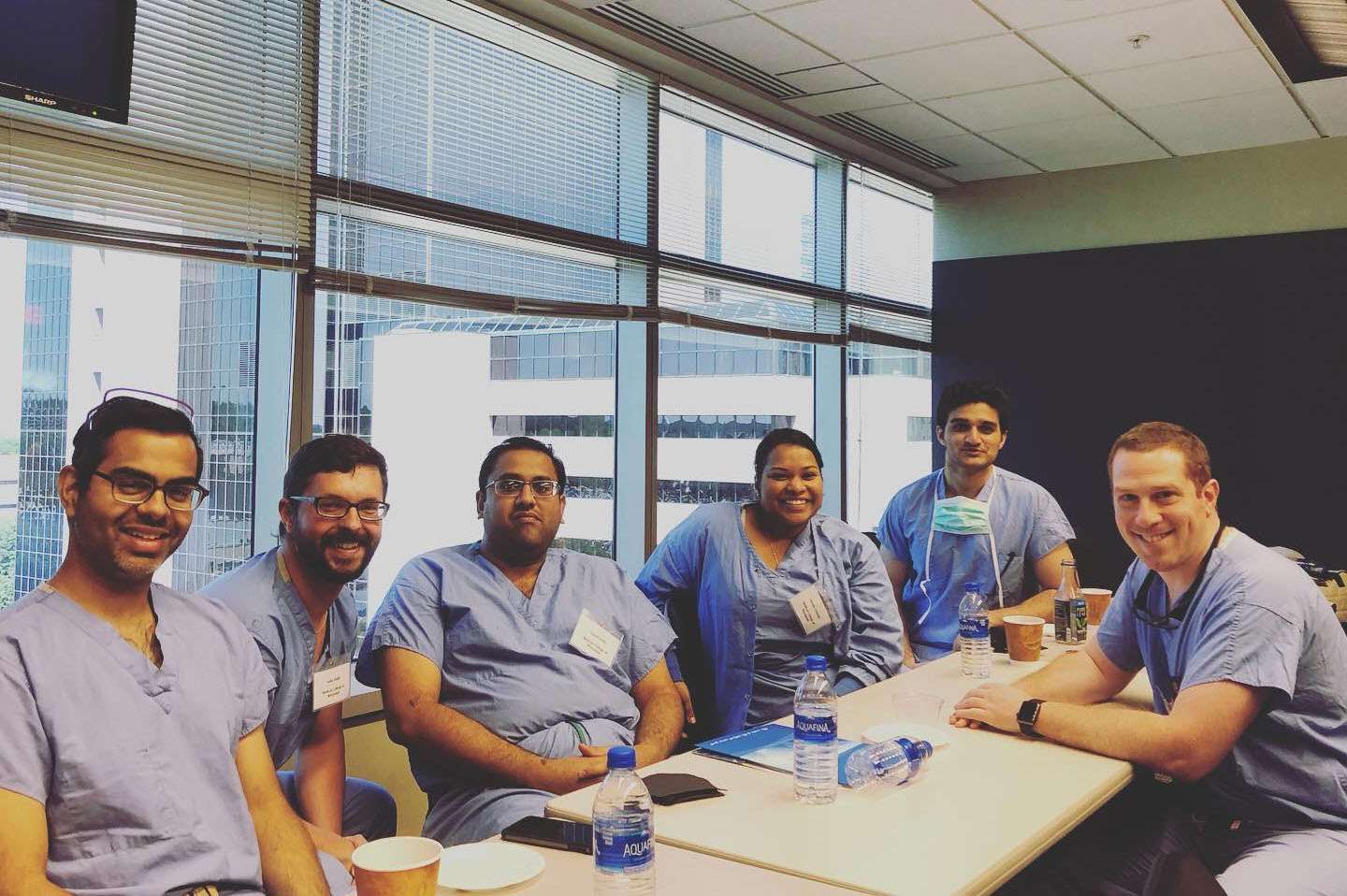
Photo Gallery
Frequently Asked Questions
Meet Our Fellows
First Year

Mansoor Burhani, MD
Pulmonary and Critical Care Fellow
Medical School: University of Illinois College of Medicine; Residency: University of Colorado
Mohammad Eshghabadi, MD
Pulmonary and Critical Care Fellow
Medical School: Caribbean Medical University School of Medicine, Curacao; Residency: Trihealth Good Samaritan Hospital, Cincinnati, OH

Joseph Pollei, MD
Pulmonary and Critical Care Fellow
Medical School: Eastern Virginia Medical School; Residency: Virginia Commonwealth University

Dre Steinwehr, MD
Pulmonary and Critical Care Fellow
Medical School: University of North Dakota School of Medicine; Residency: University of North Dakota School of Medicine
Second Year

Sushan Gupta, MD
Pulmonary and Critical Care Fellow
Medical School: University College of Medical Sciences and Guru Teg Bahadur Hospital, New Delhi, India; Residency: Carle Foundation Hospital, Champaign, IL

Karthilk Muralidharan, MD
Pulmonary and Critical Care Fellow
Medical School: Madras Medical College, Chennei, India; Residency: Bridgeport Hospital/Yale University, Bridgeport, CT

Preya Patel, MD
Pulmonary and Critical Care Fellow
Medical School: St. Matthew's University, Cayman Islands; Residency: The Wright Center for Graduate Medical Education, Scranton, PA

Hasham Saeed, MD
Pulmonary and Critical Care Fellow
Medical School: Dow Medical College, Karachi, Pakistan; Residency: Rutgers NJMS/Trinitas Regional Medical Center, Elizabeth, NJ

Karthik Seetharaman, DO
Pulmonary and Critical Care Fellow
Medical School: Arizona College of Osteopathic Medicine, Glendale, AZ; Residency: Santa Barbara Cottage Hospital, Santa Barbara, CA

Santiago Serna, MD
Pulmonary and Critical Care Fellow
Medical School: University of Cincinnati College of Medicine; Residency: Medical College of Wisconsin
Third Year

Avani Mohta, MD
Pulmonary and Critical Care Fellow
Medical School: Terna Medical College, India; Residency: Carle Foundation Hospital, Champaign, IL

Lauren Sesemann, DO
Pulmonary and Critical Care Fellow
Medical School: Chicago College of Osteopathic Medicine of Midwestern University; Residency: University of Illinois at Chicago/Advocate Christ Medical Center, Oak Lawn, IL

Krupa Shingada, MD
Pulmonary and Critical Care Fellow
Medical School: B J Medical College, India; Residency: Loyola Medicine – MacNeal Hospital, Berwyn, IL

Anoosha Tauquir, MD
Pulmonary and Critical Care Fellow
Medical School: Dow Medical College, Pakistan; Residency: Cleveland Clinic Fairview Hospital, Fairview Park, OH
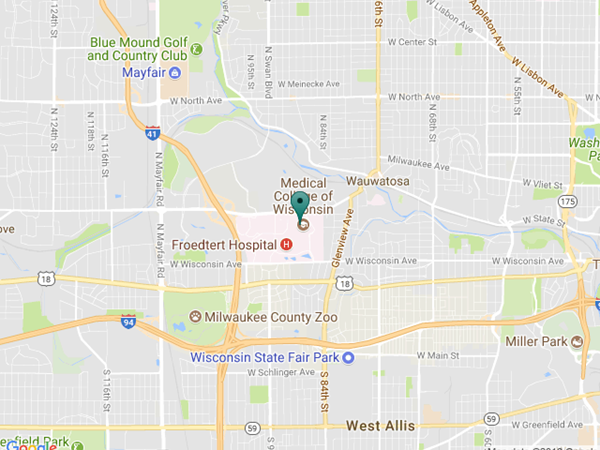
Contact Us
Pulmonary and Critical Care Fellowship
Medical College of Wisconsin
Hub for Collaborative Medicine, 8th Floor
8701 Watertown Plank Rd.
Milwaukee, WI 53226
Fellowship Coordinator
Gabby Zeinert
(414) 955-0437
(414) 955-0093 (fax)
gzeinert@mcw.edu
Program Director
Rose Franco, MD
Professor of Medicine
Division of Pulmonary, Critical Care & Sleep Medicine
rfranco@mcw.edu
Associate Program Director
Rahul Nanchal, MD
Professor of Medicine
Division of Pulmonary, Critical Care & Sleep Medicine
rnanchal@mcw.edu