Presurgical Mapping with Functional MRI (fMRI)
Surgical removal of an epileptic focus or network is an effective treatment for drug-resistant epilepsy, however people who undergo surgery on the language-dominant (typically left) hemisphere are at risk for developing new language and verbal memory deficits. The intracarotid anesthesia (Wada) test has been in use for over 50 years as a standard test of hemispheric language dominance prior to surgery. This test is invasive, however, and carries a small risk of serious complications such as infection and stroke. Soon after the discovery of fMRI in 1991, researchers in the Language Imaging Laboratory at MCW, led by Jeffrey Binder, MD, began to investigate fMRI as an alternative to the Wada test for determining language dominance (Figure 1).
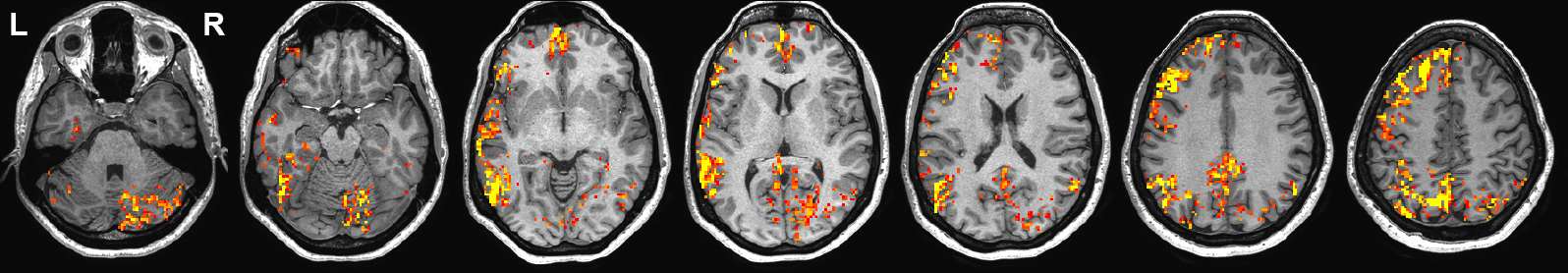
Figure 1. Example fMRI language map in a patient with temporal lobe epilepsy, using a contrast between semantic decision (language comprehension) and tone decision (sensorimotor control) tasks. The image shows typical left-lateralized activation in prefrontal, temporal, and parietal cortices, with accompanying right-lateralized activation in the cerebellum.
Supported by over 20 years of funding from the NIH, this work led to the first direct comparison between fMRI and Wada language lateralization methods (Binder et al., 1996), the first demonstration that presurgical fMRI can be used to estimate risk of language decline from temporal lobe epilepsy (TLE) surgery (Sabsevitz et al., 2003), and the first demonstration that presurgical fMRI can be used to estimate risk of verbal memory decline from TLE surgery (Binder et al., 2008) (Figure 2).
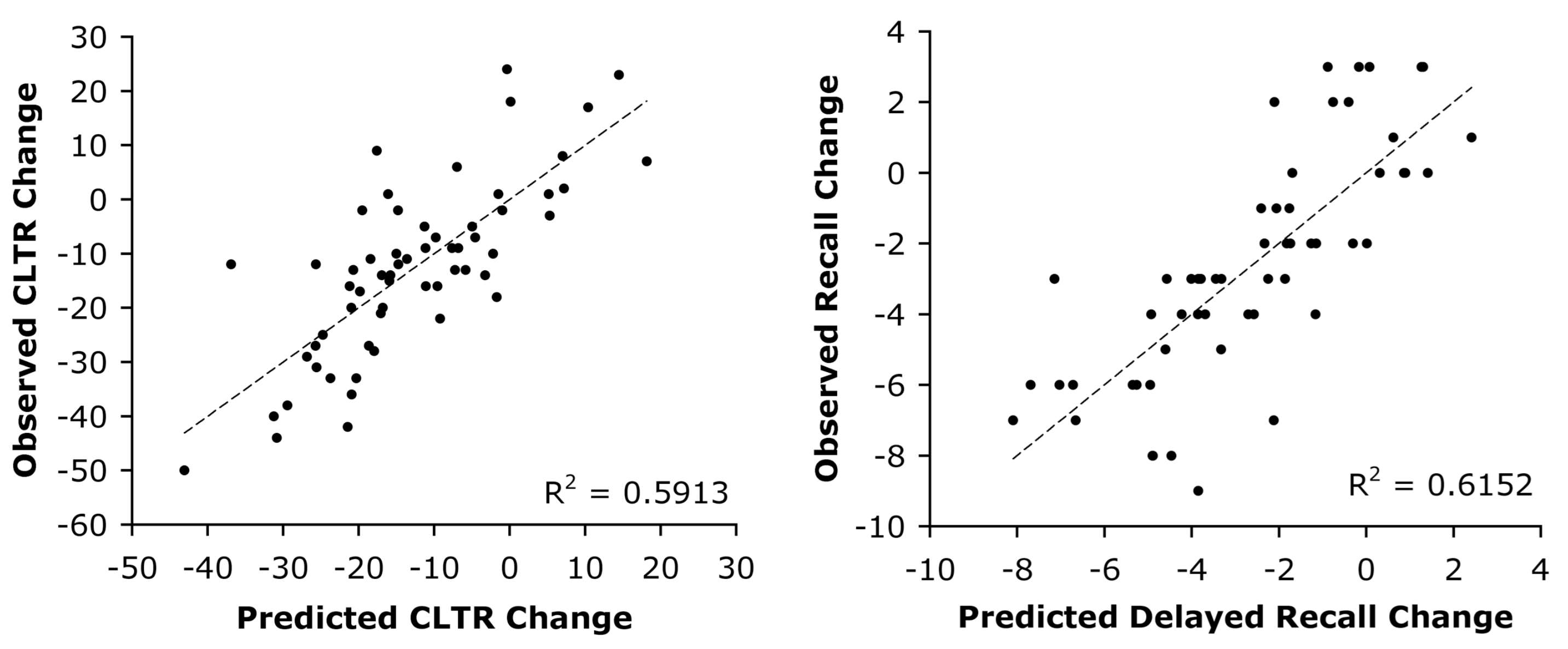
Figure 2. Multivariate Verbal Memory Outcome Prediction. Predicted compared to observed pre- to postoperative change scores on 2 verbal memory (word list memorization) tests in 60 patients who underwent left temporal lobe resections for intractable temporal lobe epilepsy. The models combine preoperative test score, fMRI language laterality index, and age at epilepsy onset as predictors.
Other landmark work included the largest fMRI-Wada comparison study by far to date (Janecek et al., 2013b), two large studies examining individual factors associated with language dominance (Springer et al., 1999; Stewart et al., 2014), and the only study to date comparing prediction accuracy in patients with discordant fMRI and Wada results (Janecek et al., 2013a). This work has made MCW Neurology a clear leader in the field of presurgical fMRI mapping and played a major role in the acceptance of fMRI as a standard clinical test in this setting (Hart et al., 2007; Szaflarski et al., 2017).
In 2012, we formed the FMRI in Anterior Temporal Epilepsy Surgery (FATES) consortium with 9 other collaborating epilepsy centers (Cleveland Clinic, Emory University, Medical University of South Carolina, University of Alabama, UCLA, University of Cincinnati, University of Rochester, University of Washington, and Vanderbilt University) to accelerate research on people undergoing left TLE surgery and to validate our methods across centers and imaging platforms (including GE, Siemens, and Philips scanners). Analysis of this dataset is underway, with preliminary results confirming our earlier observations. As part of this protocol, postoperative MRI scans were also obtained to precisely characterize the location and extent of the surgical resections. An analysis of these images led recently to a novel discovery that language decline from TLE surgery can be reduced or eliminated, even in people with left hemisphere language dominance, by limiting the posterior extension of the resection along the basal temporal lobe (Binder et al., 2020) (Figure 3). We expect this finding to have a substantial impact on defining optimal surgical approaches for medication-resistant TLE.
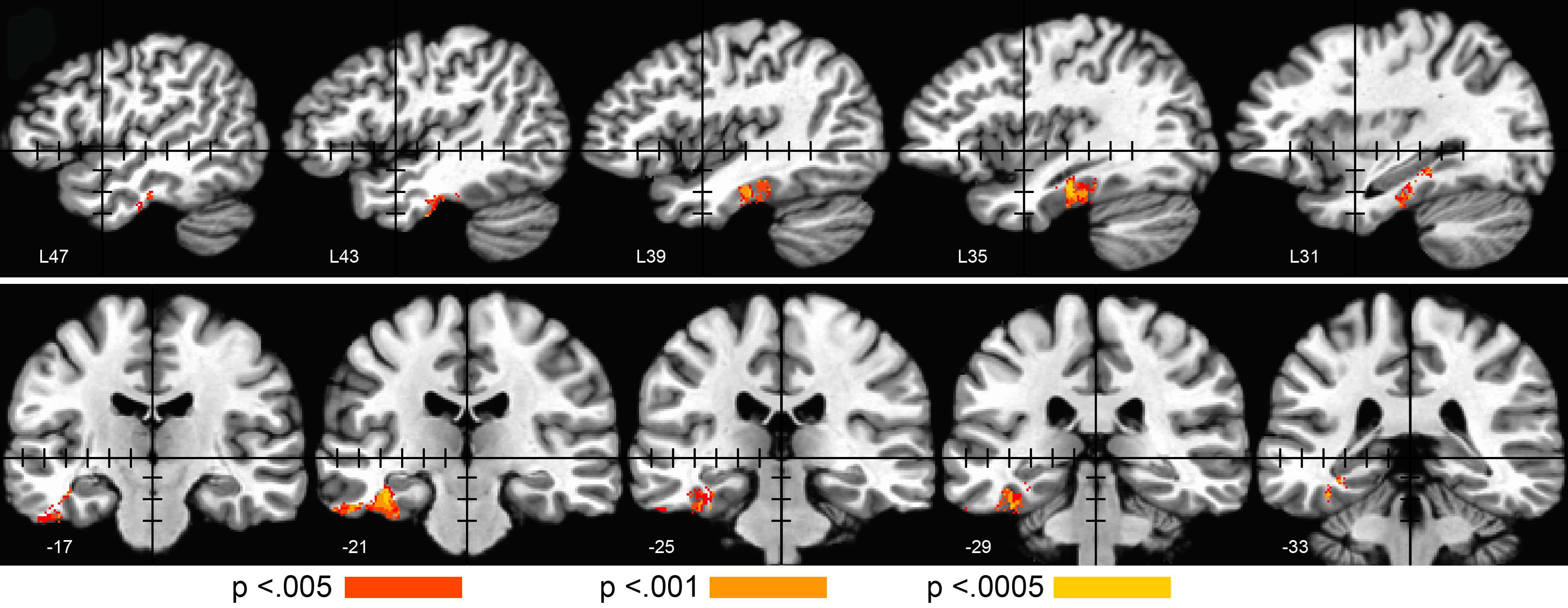
Figure 3. Voxel-based lesion-symptom mapping in 59 patients with TLE and left hemisphere language dominance, showing voxels where surgical resection was significantly related to postoperative decline in picture naming. Stereotaxic coordinates are given at the lower left of each image. Black tick marks indicate 10- mm intervals on axes centered at the stereotaxic origin.

