The Future of Drug Treatment

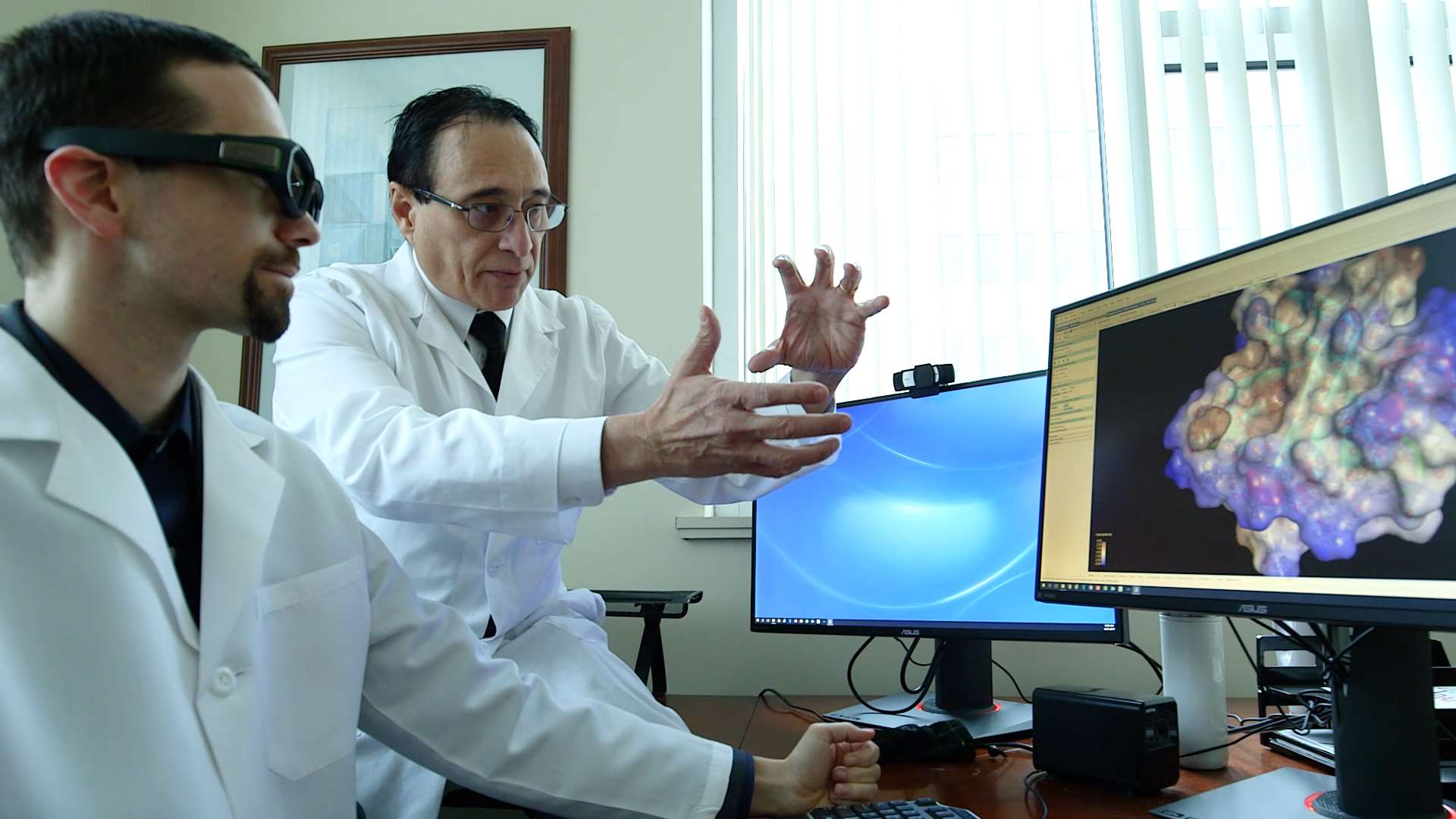
Everyone’s genetic makeup is different, but many treatments, especially medications, are similar. Clinicians and scientists at the Medical College of Wisconsin (MCW) are currently conducting research that could address this issue by leading the charge toward “precision medicine.”
The concept of precision medicine takes into consideration variations between individuals’ genomes, lifestyles and exposure to environments in order to “diagnose with precision, predict with precision and cure with precision,” says Raul Urrutia, MD, professor of surgery, Warren P. Knowles Professor of Genomics and Precision Medicine and director of the Genomic Sciences and Precision Medicine Center (GSPMC) at MCW.
Dr. Urrutia oversees the work of the GSPMC, which is conducting research in a wide range of fields, including cancer genomics, clinical genomics, obesity, biological diseases and the emerging field of pharmacogenomics.
Pharmacogenomics, the study of how genes impact an individual’s response to medications, is the best example of what precision medicine can do, Dr. Urrutia says. By testing a patient’s genome and cross-referencing it with the Clinical Pharmacogenomics Implementation Consortium guidelines, pharmacists will be able to predict with accuracy how a certain drug will affect a patient, including whether to increase or lower dosage amounts, and the probabilities that the medicines will produce their intended effects.
“Depending on the genome we have, a drug can have a good effect, bad effect or no effect at all,” Dr. Urrutia notes.
The treatment plans also can be geared toward helping patients’ individual health goals, says George E. MacKinnon III, PhD, MS, RPh, FASHP, founding dean and professor of the MCW School of Pharmacy. Dr. MacKinnon, who has helped develop several schools of pharmacy across the United States, believes pharmacogenomics will help health care providers manage specific desired patient outcomes in many areas, including pain management, cardiology, psychiatry and cancer treatments.
“When you go to the dentist, they don’t pull a crown off the shelf for you; they are custom made,” Dr. MacKinnon notes. “It makes sense that we’re beginning to realize that we need to apply this concept to patient care by personalizing medications that patients take.”
Pharmacogenomics will push pharmacists to the front lines, adds Dr. MacKinnon, as they have the knowledge and skills to interpret results and determine what medications are needed to help patients meet their goals. Ten years ago, Carolyn Oxencis, PharmD, BCPS, BCOP, clinical assistant professor at MCW and hematology/oncology clinical pharmacist at the Froedtert & MCW Clinical Cancer Center, helped implement pharmacist-conducted admission medication histories and discharge counseling at Froedtert Hospital.
Pharmacogenomics is an evolution of that work and will require a patient’s electronic medical record to expand in order to house pharmacogenomic information and develop alerts for providers.
“The pharmacist will be the first person they will go to and ask what those alerts mean,” Dr. Oxencis says.
Having more information available to create personalized medicine plans won’t be able to take away all the uncertainty that a medicine might not work, she acknowledges, but it will make the process much safer, reducing possible side effects, adverse events and toxicities.
Dr. Oxencis and other researchers at MCW are currently involved in a project to look at how breast cancer cells are reacting to certain drugs. Tracking the results of those clinical trials and creating interdisciplinary teams to use the pharmacogenomic data it derives could help put MCW at the forefront of current cancer research being conducted around the world, according to Dr. Oxencis.
Mahfoud Assem, PharmD, PhD, MCW associate professor of biopharmaceutical sciences, is also conducting research where pharmacogenomics is a key aspect. He is exploring glioblastoma, or central nervous system tumors. These rare and highly damaging tumors originate in the brain and are extremely difficult to treat, explains Dr. Assem.
“The outcomes for patients are extremely poor. The tumors don’t respond well to treatment,” he adds.
His team’s research seeks to examine genetic profiles of glioblastoma patients in hopes they can find biomarkers that will help providers predict which patients will react better to certain drugs.
“Precision medicine utilizing pharmacogenomic data could help us treat them much more effectively,” Dr. Assem says.
All these efforts are part of an ever-growing focus on pharmacogenomics at MCW. Pharmacogenomics is also an integral part of the MCW School of Pharmacy curriculum.
“While developing our curriculum to educate the pharmacist of the future, the MCW School of Pharmacy focuses on providing students with longitudinal exposure to pharmacogenomics to prepare them to practice in this emerging field,” says Dr. MacKinnon. The School of Pharmacy is a close partner of the GSPMC, providing additional educational opportunities in the areas of genomic sciences and pharmacogenomics for both current students and practicing health care providers.
These developments bode well in terms of MCW continuing to be a leader in health care research and the emerging field of precision medicine, says Dr. Urrutia. The GSPMC is already serving southeastern Wisconsin including the Froedtert & MCW health network and Children’s Hospital of Wisconsin, but by next year the plan is to service the entire state and eventually the nation, he says.
The pharmacogenomics service line in the GSPMC is led by Ulrich Broeckel, MD, professor of pediatrics, chief of the Section of Genomic Pediatrics and associate director for the GSPMC at MCW. An international researcher in pharmacogenomics for the past decade, he is leading efforts that bring together faculty from the MCW School of Medicine and School of Pharmacy as clinical applications are made available from pediatric to adult patients. Dr. Broeckel firmly believes that pharmacists are well suited to lead in this effort.
“It’s going to change everything. An analysis of your genome will become a normal part of going to the doctor,” Dr. Urrutia says.
Dr. MacKinnon echoes this sentiment: “The accessibility of pharmacists throughout our communities will help bring pharmacogenomics to patients at the local level. This will allow patients to achieve the goals of individualized medications based on their genetics, with fewer side effects and ultimately less cost to the entire health system.”
Featured in this story

George E. MacKinnon III, PhD, MS, RPh, FASHP, FNAP
Founding Dean and Professor

Raul A. Urrutia, MD
Professor, Department of Surgery; Director, Linda T. and John A. Mellowes Center for Genomic Sciences and Precision Medicine

Carolyn Oxencis, PharmD, BCPS, BCOP
Clinical Associate Professor, Department of Clinical Sciences

Mahfoud Assem, PharmD, PhD
Associate Professor, Department of Biopharmaceutical Sciences




