Medical College of Wisconsin Pathology & Laboratory Medicine


Education
The department plays a significant role in MCW's educational efforts at all levels, including undergraduate, graduate and postgraduate, as well as in the education of our peers.
Learn about our education programs
MCW Tissue Bank
The Medical College of Wisconsin (MCW) Tissue Bank is an institutional core providing research services related to human specimens to faculty investigators.
Learn about the MCW Tissue Bank
Annual Midwestern Conference
This three-day course will provide a comprehensive and practical update of diagnostic surgical pathology, with a special focus on women’s health pathology.
Learn about our conferenceWelcome from the Chair, Steven H. Kroft, MD
The Merriam-Webster Dictionary defines “Pathology” as “the study of the essential nature of diseases and especially of the structural and functional changes produced by them.” Since it also defines “Medicine” as “the science and art of dealing with the maintenance of health and the prevention, alleviation, or cure of disease,” it is not hard to appreciate that Pathology is an essential, foundational discipline for the entire practice of medicine. This applies equally to clinical care, biomedical research, and medical education.
It has been estimated that 70% of medical decisions are dependent on lab results, and Pathologists and the Clinical Laboratory Scientists with whom they work in integrated teams are responsible for all of those lab results. This encompasses everything from microscopic analysis of tissue biopsies and organ resections to innumerable blood tests to next generation sequencing of the genome. It is no exaggeration to say that modern patient care would grind to a halt without us. And, contrary to popular stereotypes, we do not hide in our offices tossing diagnostic results “over the fence” to our clinical colleagues. Instead, we are integral members of the multi-disciplinary care-giving team, providing consultation on the proper ordering and interpretation of laboratory tests, as well as critical pathological information to drive management decisions in this age of increasingly personalized medicine. We are also skilled in quality management and improvement, process improvement, and systems management, allowing us to serve as leaders in our healthcare systems.
 In the area of medical research, we are the experts in the handling of tissue and other biological specimens, as well as in the laboratory techniques to extract information from them. Whether in the realm of basic science, translational research, or clinical research, we have the knowledge and skills to add new information to the medical literature on the mechanisms, classification, diagnosis, and management of essentially every human disease, either as independent investigators or as indispensable collaborators with other researchers.
In the area of medical research, we are the experts in the handling of tissue and other biological specimens, as well as in the laboratory techniques to extract information from them. Whether in the realm of basic science, translational research, or clinical research, we have the knowledge and skills to add new information to the medical literature on the mechanisms, classification, diagnosis, and management of essentially every human disease, either as independent investigators or as indispensable collaborators with other researchers.
Finally, pathology is a fundamental component of medical education; without a thorough grounding in pathology, physicians cannot achieve a deep understanding of the diseases they are responsible for treating. And pathology education doesn’t stop with second year medical students. We serve as educators through the entire lifecycle of medical practice, from Undergraduate Medical Education to Graduate Medical Education to Continuing Medical Education, for a broad range of medical professionals.
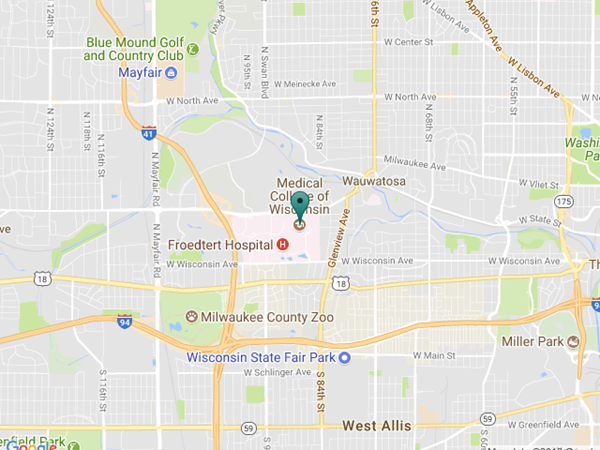
Contact Us
Medical College of Wisconsin
Froedtert/Medical College Lab Building
FMCLB 226
9200 W. Wisconsin Ave.
Milwaukee, WI 53226-3522
(414) 805-6980 (fax)