Medical College of Wisconsin Otolaryngology Residency Program
- Positions Available Per Year: 4, 3, 4, 3, 4 (4 positions will be offered in the 2025 Match)
- Years of Training: 5
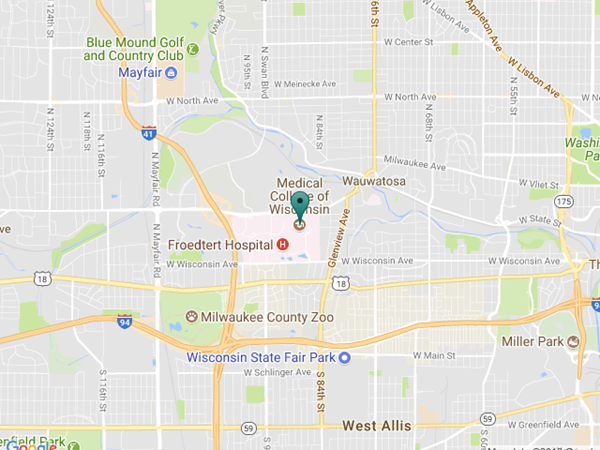
- Locations: Froedtert Hospital, Children's Wisconsin, Clement J. Zablocki VA Medical Center, and Froedtert Hospital Menomonee Falls
- Program Director: Thomas Robey, MD
- Associate Program Director: Lauren North, MD
- Residency Coordinator: Diann Fiscus
dfiscus@mcw.edu
(414) 955-0827 | (414) 955-0074 (fax)
Follow us on Instagram @mcwoto

2026 Resident Applicant Announcement
MCW Program will match 4 residents in 2026
The otolaryngology residency program at the Medical College of Wisconsin-Milwaukee (MCW) was recently granted a complement increase by the Accreditation Council for Graduate Medical Education (ACGME). Beginning with the next match cycle, the program will accept 4 new residents per year, reaching and maintaining a full complement of 20 residents by the 2029–2030 academic year.
- Resident Applicant Interviews will be held December 12 & 13, 2025.
- Interview offers will be distributed November 6, 2025.
- Interview acceptance date is November 10, 2025.
ENT Residency at MCW - Video Presentation
Hear from our residents about what it's like to be an otolaryngology resident at MCW.
Message from the Program Directors

Thomas C. Robey, MD
Professor
Pediatric Otolaryngology & Residency Program Director
Medical College of Wisconsin

Lauren M. North, MD
Assistant Professor
Rhinology and Sinus Surgery & Associate Program Director
Medical College of Wisconsin
Resident Spotlight: Stefan Vidovich, PGY3
Keeping Wellness Initiatives Alive
Reasons to live in Milwaukee
About the Program
Training Overview
The Department of Otolaryngology and Communication Sciences at the Medical College of Wisconsin (MCW) provides residents with a superior, quality education in an academic setting.
The Department features a very sizeable and diverse group of specialty trained otolaryngologists, representing all facets of the specialty. Faculty are nationally and internationally recognized, and are amongst the leaders in the field of otolaryngology as well as their respective sub-specialties.
In addition, the Department has a robust Division of Research, receiving almost $4,000,000 of external funding annually.

Mission Statement
The mission of the Department of Otolaryngology and Communication Sciences Residency Program is to produce superbly trained otolaryngologist-head and neck surgeons who provide exceptional patient care and are future leaders, researchers, and educators in otolaryngology. This mission aligns with that of the Medical College of Wisconsin to promote excellence in patient care, innovation, research, and education in an academic environment. The residency program strives to define the future of otolaryngology-head and neck surgery through core values of compassion, professionalism, integrity, and excellence.

Program AIMS
The Otolaryngology Residency Program at MCW aims to:
• Develop residents into well-rounded clinicians who practice evidence-based medicine and exhibit high-quality surgical skills in all areas of otolaryngology.
• Prepare future leaders, researchers, and educators in otolaryngology.
• Provide and support a training experience that will allow graduates to choose their own specialty career path.
• Establish an environment committed to promoting a healthy work-life balance and life-long learning.

Resident Experience
Otolaryngology residents train at four different hospitals, each offering a unique perspective on patient care.
The main teaching institution, Froedtert Hospital, is a 585-bed tertiary care facility serving all Southeastern Wisconsin. Located on the same campus, Children’s Wisconsin is the oldest and largest children’s hospital in the state and is one of the busiest children’s hospitals in the country. The Clement J. Zablocki VA Medical Center, located a few miles from the main campus, offers trainees the unique opportunity to care for our nation’s veterans. Finally, located 15 miles from the main campus, Froedtert Menomonee Falls Hospital provides residents the experience of working in a community-based hospital.
With the abundant opportunities available, otolaryngology residents receive a well-rounded education with excellent clinical and operative experience allowing graduates to choose their own specialty career paths.

Learn more about our residency program including rotation schedule details, duty hours, conferences, call specifics and more.

Residency Photos
Contact Us
Otolaryngology and Communication Sciences
Clinical and General Information
(414) 955-0830
slistinsky@mcw.edu