Project LEAD: Laws to End Abuse and Diversion
Specific Aims of the Project
2.) Identify how local implementation of state laws and policies may contribute to the transition from nonmedical prescription opioid use to injecting prescription opioids or injecting heroin or using fentanyl.
3.) Compare local factors in urban, suburban and rural areas that affect the riskiness of injection practices such as the availability of clean syringes, diffusion of norms, injection practices and perceptions of laws to reduce opioid misuse in drug using networks and accessibility of drug treatment programs.
Dangers of Opioids
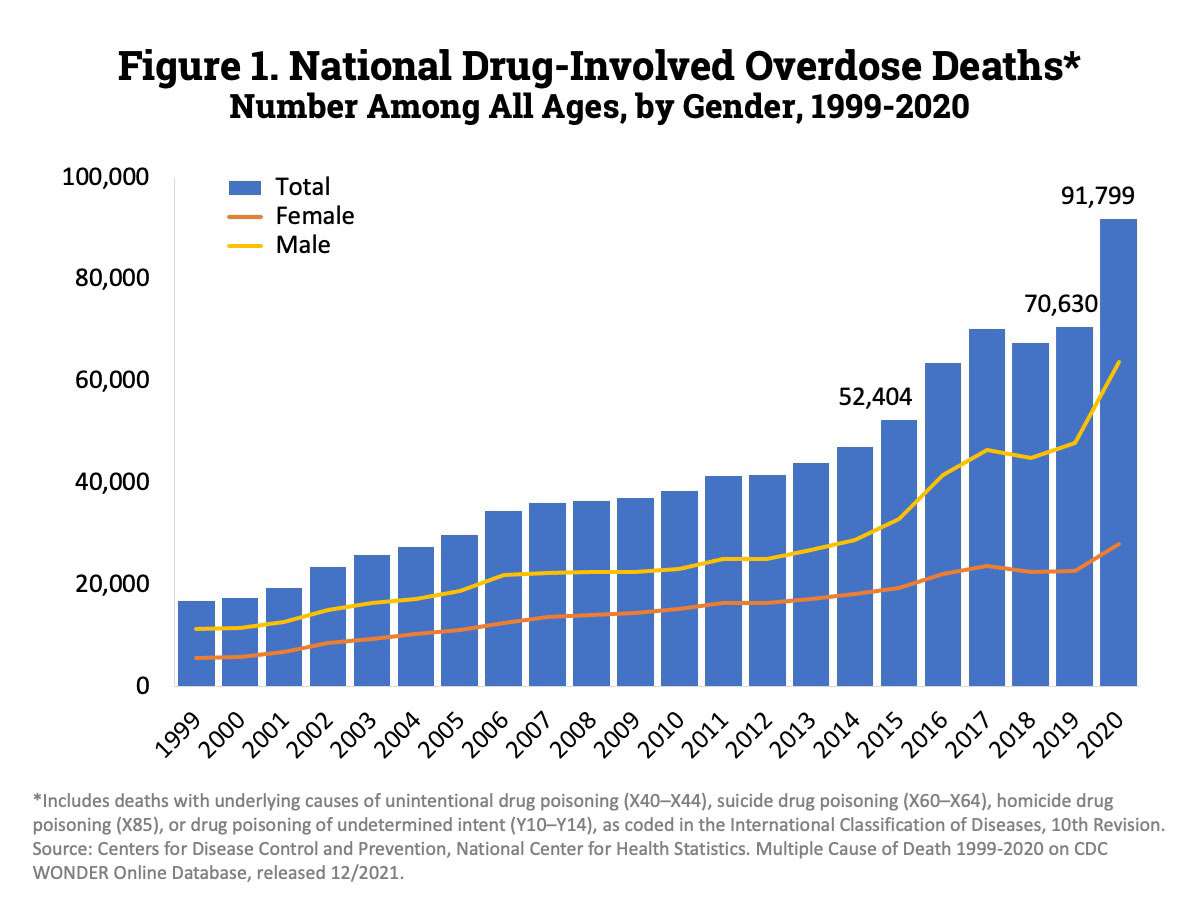
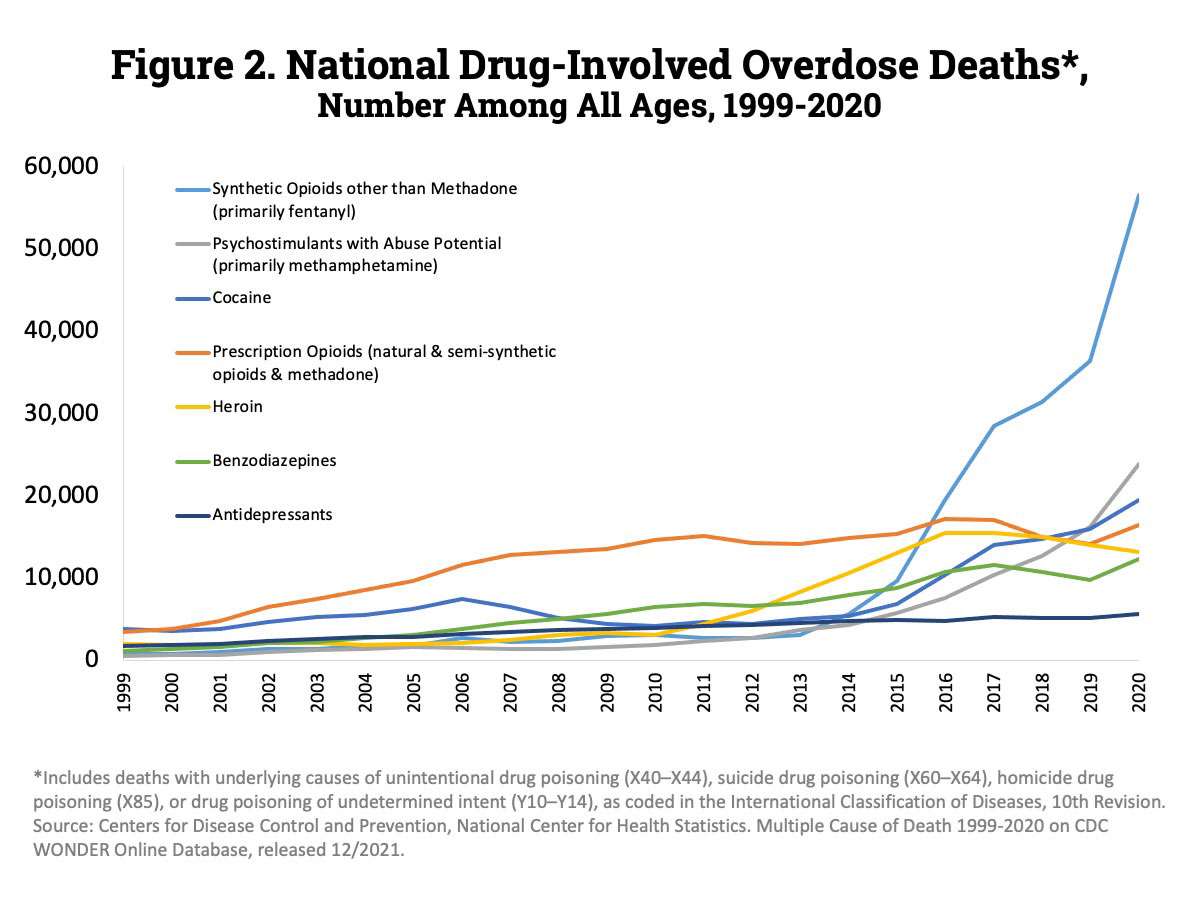
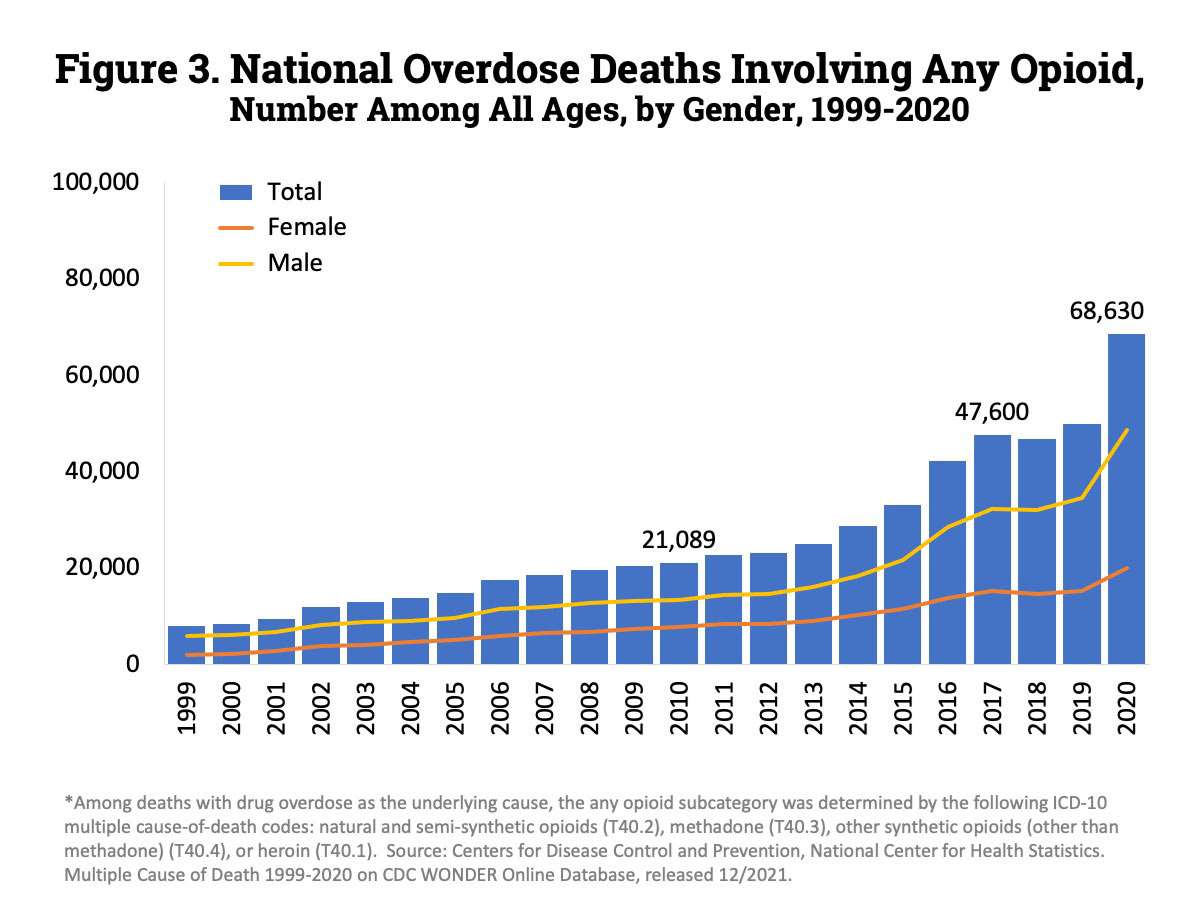
Drug Overdose Death Rates
Source: National Institute on Drug Abuse; National Institutes of Health; U.S. Department of Health and Human Services.
About the Project
It is essential to understand the conditions that facilitate transition from oral prescription opioid use to injection of prescription opioids, heroin, and fentanyl. In response to rising rates of opioid dependence and fatal poisonings, virtually every US state has incorporated laws to reduce the availability of medical opioids for diversion. However, little research has examined the effects of these laws on the transition to injecting opioids, or using heroin, or fentanyl.
Forty-nine states have implemented prescription drug monitoring programs (PDMPs) which are state-based data collection systems that record controlled medications. However, state PDMPs differ considerably, including the extent to which physicians are required to access PDMPs before prescribing opioids. The effects of different PDMP systems on the transition to injection drug use or heroin or fentanyl use is not clear. PDMPs may make prescription opioids more expensive or harder to obtain, leading to injecting these substances to produce the same effects, or turning to heroin or fentanyl. On the other hand, decreased opioid availability may decrease initiation of non-medical opioid use and consequently decrease transition to injection, or heroin or fentanyl use.
Other laws states have introduced to help decrease the diversion of prescription opioids include regulation of pain clinics. Medicaid and private insurance companies, that also vary by state, have implemented practices to detect “doctor shopping” and excessive prescription of opioids and to reduce prescription opioid misuse that might affect transition to opioid injection or heroin or fentanyl use. State Medicaid policies also play a role in patients’ access to and use of Medication Assisted Therapy (MAT) such as buprenorphine or methadone. Such policies may increase or reduce the accessibility of MAT and increase the probability of injection.
Finally, features of the local context may increase the probability of transitioning to injecting prescription opioids or heroin or fentanyl, and may contribute to the riskiness of injection practices including the relative price and quality of heroin/fentanyl compared to prescription opioids and the relative density and size of social networks. In some urban areas, heroin markets may be well-established and heroin or fentanyl may be less expensive relative to prescription opioids. Rural and suburban areas may not have ready access to syringe exchange programs (SEPs), sterile syringes from pharmacies or other harm reduction or prevention services such as hepatitis vaccination.
Research Focus
This research will explore the influence of laws in three different states, Connecticut, Kentucky and Wisconsin, selected to represent differences in PDMPs, Medicaid restrictions on opioid prescription, and pain clinic regulation. We will also examine the effects of the local context (drug use networks, syringe availability, harm reduction services relative price and quality of heroin) on the transition to injecting non-prescription opioids and /or heroin injection or fentanyl use in three local areas, an urban area, a smaller metropolitan area or suburb, and a rural town and surrounding county, chosen to reflect areas with higher rates of opioid prescription.
Resources

-
211 Guided Search for Treatment
Learn More -
SAMSHA Treatment Locator
Learn More -
Never Use Alone
Learn More -
Dose of Reality (search for places to get Narcan and fentanyl test strips for free)
Learn More -
211 Needle Exchange Locator
Learn More
Publications and Presentations
Dickson-Gomez, J., Spector, A., Weeks, M., Galletly, C., McDonald, Green, D. Epub ahead of print. “You’re not supposed to be on it forever”: Medication Assisted Therapy (MAT) Related Stigma among drug treatment providers and other medical professionals. Substance Abuse: Research and Treatment
Dickson-Gomez, J., Spector, A., Krechel, S*, Li, J., Montaque, H. D. G., Ohlrich, J., Galletly, C., Weeks, M. In press. Barriers to drug treatment in police diversion programs and drug courts: A qualitative analysis. American Journal of Orthopsychiatry
Dickson-Gomez, J., Spector, A., Ohlrich, J., and Christiansen, E. A systems analysis of Milwaukee’s response to the opioid crisis. Oral presentation, Contemporary Drug Problems, Prato, Italy, 09/2019.
Dickson-Gomez, J., Krechel, S*, Spector, A., Weeks, M., Ohlrich, J., Montaque, H.D.G., Li, J. In press. The effects of opioid policy changes on transitions from prescription opioids to heroin, fentanyl and injection drug use: A qualitative analysis. Substance Abuse Treatment and Research
Dickson-Gomez, J., Weeks, M., Green, D., Boutouis, S., Galletly, C., Christenson, E. Epub ahead of print. Insurance barriers to substance use disorder treatment after passage of mental health and addiction parity laws and the Affordable Care Act: a qualitative analysis. Drug and Alcohol Abuse Reports
Dobbs, J., and Dickson-Gomez, J. Rural, suburban, and urban access to sterile injection equipment and syringe services programs. Poster presentation, MCW M3 Scholarship Forum, In Person, 6/2022
Montaque, H. D., Christenson, E., Spector, A., Wogen, J., McDonald, M., Weeks, M. R., Li., J., & Dickson-Gomez, J. (2022). Mechanisms for expanding harm reduction for opioid use in suburban and rural US settings. Journal of Drug Issues. DOI:10.1177/00220426221108694.
Ohlrich, J., Dickson-Gomez, J., Christiansen, E. “Keeping people out of jail in regards to drugs is a collaborative effort”: Public health and criminal justice collaboration in Milwaukee County Adult Drug Treatment Court. Oral presentation, Contemporary Drug Problems, Prato, Italy, 09/2019
Ohlrich, J., Dickson-Gomez, J., Christiansen, E. “Keeping people out of jail in regards to drugs is a collaborative effort”: Public health and criminal justice collaboration in Milwaukee County Adult Drug Treatment Court. Poster presentation, Virtual Research Week, Medical College of Wisconsin, Virtual, 02/2021.
Spector A, Christenson E, Dickson-Gomez J. “By the time my prescription got over...I was already hooked”: A preliminary examination of women’s experiences initiating opioid misuse. Poster presentation, InWomen’s Conference, Virtual, 06/2020
Spector, A and Dickson-Gomez, J. Changes in uptake following the expansion of naloxone access laws: Perspective of key informants in Wisconsin. Oral presentation, Contemporary Drug Problems, Prato, Italy, 09/2019
Spector, A and Dickson-Gomez, J. The role of syndemic and structural factors in substance use disorder treatment-seeking among women in the United States with a history of opioid misuse: A qualitative study. Oral Presentation, InWomen’s Conference, Virtual, 06/2021
Spector A, Dickson-Gomez J. “Well, my kids always come first”: A preliminary examination of the role of children in the lives of women who misuse opioids. Poster presentation, Annual Meeting of the American Psychological Association, Virtual, 08/2020
Spector, Antoinette L., Galletly, Carol L., Christenson, Erika, Montaque, H. Danielle G., & Dickson-Gomez, Julia. (In Press). A qualitative examination of naloxone access in three states: Connecticut, Kentucky, and Wisconsin. BMC Public Health.
Spector AL, Quinn KG, deRoon-Cassini TA, Young SA, O'Brien M, & Dickson-Gomez J. (2021). Syndemics and the etiology of opioid misuse among women: A qualitative study. SSM-Qualitative Research in Health, 100028.
Spector AL, Quinn KG, Young SA, O'Brien M, deRoon-Cassini TA, & Dickson-Gomez J. (2021). A qualitative examination of substance use disorder treatment-seeking among women with opioid use disorders: The role of syndemics and structural violence. SSM-Qualitative Research in Health, 1, 100014.
National Institute on Drug Abuse (NIDA) honorable mention: “Mapping Patient Journeys in Drug Addiction Treatment Challenge”
Project LEAD Team

Julia Dickson-Gomez, PhD
Professor

Jared M. Dobbs, MPH
Medical Student

Juan Flores
Research Associate I

Carol Galletly, JD, PhD
Professor

Sarah Krechel
PhD Student

Jessica Ohlrich, MPA
Research Coordinator
Non-MCW Team
Jennifer Havens, Kristen Johnson, Jane Lynch: University of Kentucky
Antoinette Spector: UW-Milwaukee