Medical College of Wisconsin Radiation Oncology Technology and Services
The Department strives to provide exceptional patient care by delivering state of the art radiotherapy services in a compassionate, personalized, efficient and value-based manner, that is grounded by expertise and experience with the latest oncologic and radiotherapeutic principles and practices.
Equipment in the Department of Radiation Oncology
Radiation Oncology Services by Radiation Therapy Modality
The use of the latest technological advancements in high-precision Image-Guided Adaptive Radiation Therapy - including High-field MR-Linac, Radixact™ tomotherapy with Synchrony motion tracking, in room CT-on-rails, Gamma Knife ICON™, 3T MR simulation, Dual-source dual-energy CT simulation, MR guided brachytherapy - enable our faculty and staff to provide patients with precise and personalized therapy that increases tumor control, minimizes treatment side effects and improves quality of life.
MRI-Guided Adaptive Radiation Therapy (ART)
(Left: Pancreatic cancer treated with MR-guided ART)
Real-Time Motion Tracking
In collaboration with Accuray Inc., we were the first clinic worldwide to use Accuray’s Synchrony technology for real time motion tracking during radiation therapy delivery. This motion management dramatically reduces the need for large target margins which have traditionally been used to compensate for the motion. As a result, the amount of healthy tissue exposed to radiation is reduced, minimizing the incidence of side effects.
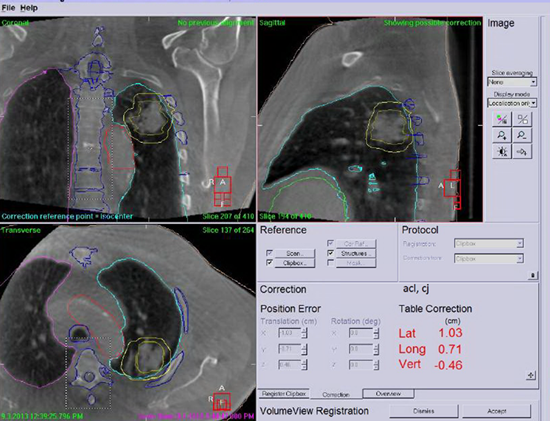
Image-Guided Radiation Therapy (IGRT)
Stereotactic Body Radiotherapy (SBRT)
At Froedtert & the Medical College of Wisconsin, the delivery of SBRT involves in 4DCT or MRI based treatment planning, online MRI or CT guidance using MR-Linac, Radixact tomotherapy, Versa HD linac with cone beam CT, or Mevion proton with CT-on-Rails, real-time motion tracking, respiration gating, and surface-guided (VisionRT) motion monitoring.
Stereotactic Radiosurgery (SRS) with Gamma Knife
Intensity Modulated Radiation Therapy (IMRT) and Volumetric Modulated Arc Therapy (VMAT)
Brachytherapy
Seed Implants (Brachytherapy for Prostate Cancer)
Radioactive "seeds" are implanted in the prostate gland, where they fight cancerous tumors for several months. One of the advantages of using this technique for prostate cancer is that it limits the dose received by normal structures and patients are not required to return for daily radiation treatments.
High Dose Rate (HDR) Brachytherapy
Brachytherapy is defined as the placement of radioactive sources directly into or close to a tumor. High radiation doses are delivered to the cancer cells with rapid fall-off in dose to normal tissues. Brachytherapy is often combined with external beam radiation therapy (EBRT), serving as a 'boost dose' to the area of suspected or gross tumor residual. Brachytherapy alone or in conjunction with other treatment modalities has become an important part of radiation treatment. HDR brachytherapy is used in our department to treat gynecological, breast, and prostate cancers. At Froedtert & the Medical College of Wisconsin, CT and/or MRI are used to plan HDR brachytherapy.
Eye Plaque Brachytherapy
Eye plaques containing radioactive seeds are used in the treatment of choroidal melanomas.





