MCW Pancreatic Cancer Patient Education & Treatment
Additional resources to help you every step of the way
Learn more in Pancreas school!
The new Pancreas School series is hosted by Dr. Douglas B. Evans, Chair of the Department of Surgery. Pancreas School will provide a primer on important topics relating to diagnosis and treatment of pancreatic cancer, highlighting the expertise of providers at the MCW LaBahn Pancreatic Cancer Program.
Watch Pancreas School EpisodesWe are Here to Help
A cancer diagnosis is a life-changing event for patients and their family members. It can be an overwhelming experience for everyone involved. On this page, we’ve gathered a number of additional resources and support materials to help you stay informed and hopeful during this difficult time.
Personalized Care Plan
Diagnosing Pancreatic Cancer
Overview
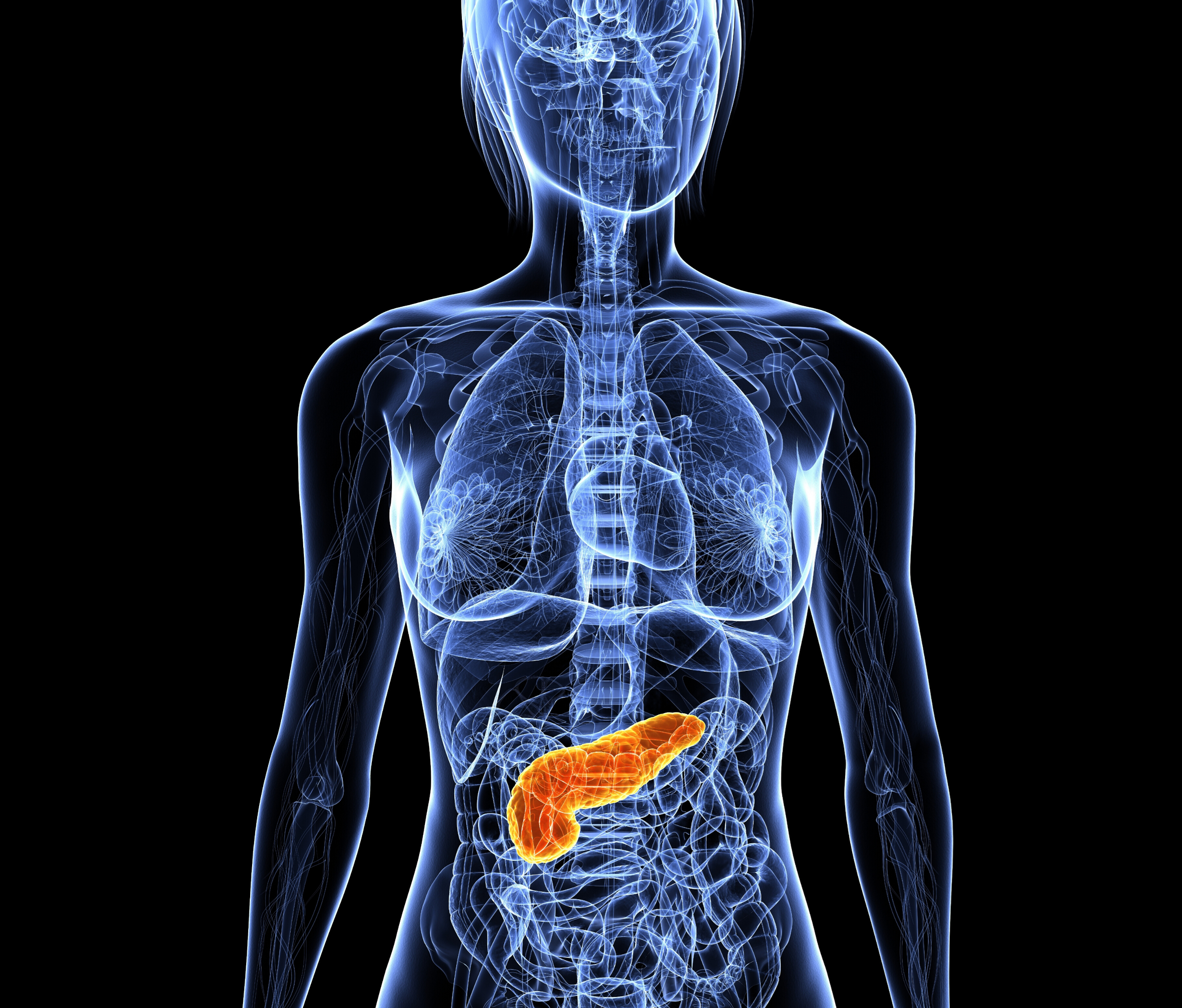
The pancreas is an organ located deep in the belly between the stomach and backbone, surrounded by the liver, small intestine and important blood vessels. The function of the pancreas is to produce pancreatic juices that contain enzymes to help breakdown food. It also makes insulin and other hormones that travel throughout the body to help the body use or store energy that comes from food. When uncontrolled cell growth occurs in the pancreas, it can form tumors that can lead to pancreatic cancer. It is important to understand which type of pancreatic cancer one has – adenocarcinoma which arises from cells that line the pancreatic ducts, or neuroendocrine which arises from endocrine cells. Signs and symptoms of pancreatic cancer may include abdominal pain, jaundice, new onset diabetes, diarrhea, and weight loss.
Imaging tests
High quality imaging tests are important to determine the location of the tumor and to define its extent. A computed tomography (CT) scan is a special type of x-ray that is used to visualize the pancreas and determine if the tumor can be surgically removed. A magnetic resonance image (MRI) uses powerful magnets and radiowaves to provide detailed pictures of the inside of the body. A positron emission tomography (PET) scan is used to identify malignant cells. A dotatate scan is only used for patients with neuroendocrine tumors and can identify these neuroendocrine cells.

Endoscopic procedures
A biopsy of the tumor is needed to help make an accurate cancer diagnosis. Endoscopic ultrasound and fine needle aspiration (EUS/FNA) is the most common procedure used to obtain a biopsy of the pancreatic tumor. This involves using a thin, tube-like Instrument to look at the inside of the body and to take a biopsy of the tumor.
Endoscopic retrograde cholangiopancreatography (ERCP) is another procedure that can be performed If you are jaundiced. Jaundice is most likely the result of a blocked bile duct by the pancreatic tumor and the ERCP helps to place a stent in order to relieve this blockage. In addition to these procedures, blood and other lab tests may be performed.

Treatment
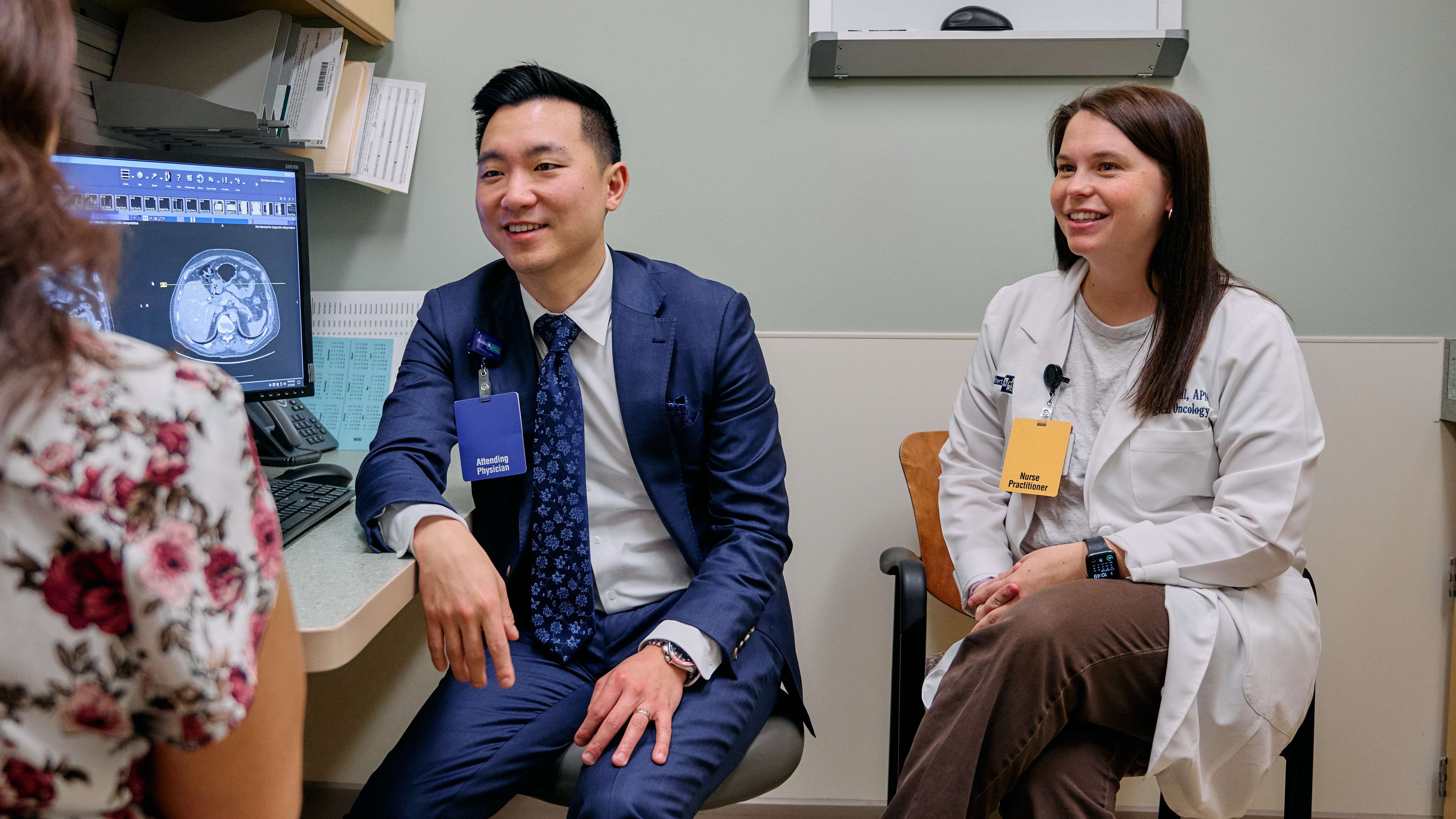
At the Medical College of Wisconsin, our physicians work to provide the best treatment for each individual’s disease
Chemotherapy
Why is it used?
Chemotherapy is a form of treatment that uses intravenous (IV) and/or oral drugs to stop the growth and multiplication of cancer cells. These drugs enter the circulation system and kill cancer cells within and outside the pancreas There are several drugs that can be used in combination to treat pancreatic cancer. Your medical oncologist will prescribe the specific chemotherapy drug combination used to treat your cancer.

How is it given?
Most chemotherapy is given via the intravenous route by specially trained nurses. Often, a port will be placed prior to starting chemotherapy. The regimen, frequency, and duration of the chemotherapy will be set by your medical oncologist. You will have a dedicated chemotherapy education session with the nurse on the medical oncology team and will be given additional written drug information for each of the drugs in your regimen.

Possible side effects
Side effects will vary per individual and are specific to the drugs administered. Not everyone will experience every side. The common side effects associated with chemotherapy include nausea, vomiting, hair loss, destruction of blood cells, diarrhea, mouth sores, numbness, and tingling of hands and feet.
Our cancer program offers the ability to talk to a nurse and doctor 24/7 if you have concerns or questions about your symptoms. While on chemotherapy, we encourage you to call with any side effects or questions you make have and we will give directions on how to proceed.

Radiation Therapy
Why is it used?
Radiation therapy is a localized type of treatment and uses high energy x-rays to kill cancer cells. It is directed at the pancreatic tumor and surrounding pancreatic tissue as well as the lymph nodes and blood vessels near the tumor. Radiation therapy is generally given prior to surgery – it makes the tumor easier for the surgeons to remove. It also decreases the chance that cancer cells will be found in the lymph nodes around the tumor. Whether radiation therapy is recommended depends on the stage of pancreatic cancer you have.

How is it given?
Radiation therapy is delivered by a computer-controlled machine which directs multiple beams of radiation through the skin to the tumor. The course of radiation therapy for each patient will be determined by the radiation oncologist.
Radiation therapy is generally given with a low dose (mild) chemotherapy. Chemotherapy can enhance the effects of radiation on the tumor. Chemotherapy is either given as a weekly infusion or as a pill taken twice daily at home.
Radiation therapy is given daily, Monday through Friday, for 5.5 weeks for some patients and in a more abbreviated course of 5-10 treatments for other patients. Radiation therapy treatment visits usually last for approximately 30 minutes. Radiation therapy does not cause pain while it is being given. You will have weekly visits with the radiation oncologist and the nurse practitioner to monitor for side effects.

Possible side effects
Side effects from radiation will vary by each individual. Some of the common side effects of radiation therapy include nausea, vomiting, heartburn/upper abdominal discomfort, increased gas production/bloating, decreased appetite, and fatigue. Side effects are temporary and usually well managed. You maybe be prescribed medications to help with these symptoms, such as antacids or nausea medications. Talk to your doctor or nurse if you are experiencing side effects.

Surgery
What is it?
Surgery is often the most challenging part of pancreatic cancer treatment. During surgery, your surgeon will remove the pancreatic tumor and take a biopsy of any other tumors you may have. This will be sent to pathology to determine the AJCC (pathologic) stage of your pancreatic cancer. Your surgeon will discuss your pathology results with you when they become available and give recommendations for any additional therapy. Your surgical team will have a detailed discussion with you about what to expect during the post-operative period. Recovery from surgery generally takes about two months, and the stronger a patient is going into surgery, the more rapidly they will recover. Therefore, even before surgery, we emphasize the importance of nutrition and physical activity. We encourage you to take advantage of our dietitians and physical therapists throughout the course of treatment.

Types of surgery
Depending on the location of the tumor, different surgical operations may be recommended.
- A laparoscopy is when a surgeon uses a small camera to look inside the abdomen to find small tumors outside of the pancreas.
- Whipple (Pancreaticoduodenectomy) is a procedure that involves removing the head of the pancreas, along with the bile duct, gallbladder, the upper part of the intestine, and part of the stomach.
- Distal pancreatectomy is often performed to remove tumors of the body and tail of the pancreas; this may include removal of the spleen.
- Total pancreatectomy is performed to remove the whole pancreas, part of the stomach, small intestine, the common bile duct, gallbladder, spleen, and nearby lymph nodes.
- Bypass procedure may be performed if removal of the tumor is not recommended, but the tumor is causing blockage of the bile ducts or intestines. This procedure helps to reroute the bile duct and stomach around the area of obstruction.

Surgery recovery
Most patients stay in the hospital for about 7-10 days after surgery. During this time, patients participate in physical therapy, slowly resume their diet, meet with a registered dietitian to discuss nutritional goals, start taking pancreatic enzyme supplements and antacid medications, and have blood sugars monitored.

Research & Clinical Trial Options
Other Treatment Opportunities
At the Medical College of Wisconsin, we are dedicated to providing the best care as possible to our patients. We strive to give our patients as many treatment opportunities are we can. Clinical trials and research are just one way we are dedicated to optimizing pancreatic cancer treatment. Click on the side bars to learn more about other treatments opportunities.

Research
The LaBahn Pancreatic Cancer Program is committed to translating research into cutting-edge treatments for our patients. Scientists from the program store donated tissue, blood, and health information from our patients. The goal of this is to improve healthcare and develop new treatments for cancer. Participation in any of our research is completely voluntary.

Clinical Trials
A clinical trial is a type of research study that tests how effective new medical approaches are in comparison to standard therapy. These are one of the most powerful ways that your doctors can learn how to best treat your pancreatic cancer. At the Medical College of Wisconsin, we are committed to the advancement of clinical trials. We have dedicated infrastructure for clinical research and the region’s only Translational Research Unit, designed just for patients participating in early phase (phase I/II) clinical trials. As our laboratory research leads to important new targets in cancer, a dedicated unit to perform cancer treatment trials makes these promising treatments available to patients sooner. Ask a doctor for more information about clinical trials options.

Supportive Care
Endocrine
It is not uncommon for patients with pancreatic cancer to experience high blood sugars. Usually the goal blood sugar is between 80 and 130 mg/dl before a meal and no greater than 180 mg/dl two hours after eating. Hemoglobin A1C is a test that tells your medical team how much sugar has been in your blood over the past two to three months. If your blood sugar level is higher than it should be, your medical team may ask you to see a diabetes specialist who will work closely with you to tailor your medications to ensure good control of high blood sugars. Good blood sugar levels are very important for healing, preventing weight loss and dehydration.

Nutrition
Pancreatic cancer may cause significant nutritional challenges. Upon diagnosis, a consultation with a registered dietitian can provide a platform for a nutritional assessment and meal planning. It is important that you understand the importance of consuming a diet rich in protein, calories, vitamins and minerals. Hydration is also an important component of any nutrition plan. Goal setting based on your needs may include weight management (either to regain weight loss or maintain current weight), symptom management (prescribing medications to help with nutritional challenges), nutrition education and meal planning. Empowering you with nutrition knowledge is vitally important to meeting your personal nutrition goals set forth.

Psychosocial Support
All patients with pancreatic cancer have access to appointments with our team’s psychologist. Behavioral health treatment and counseling can help you cope with stress, difficult feelings, and the challenges of committing to lengthy treatment protocols. Diagnosis of and treatment for pancreatic cancer can be stressful, upsetting, and present challenges for practicing good self-care. You may experience worry about your health, your family members, work, and finances. You may experience sadness about your diagnosis and how it impacts the activities you are able to engage in. You may also run into challenges coping with treatment, including tolerating discomfort, and maintaining healthy sleep. . Talking with a trained psychologist and receiving adequate support can help address these concerns and may improve your ability to succeed during and after treatment.

Wellness
Small Stones Wellness Center supports the treatment and healing process by enhancing patients’ appearance, boosting their self-esteem, and promoting optimal health and well-being. While you concentrate on your health, let skilled and compassionate staff help you look good and feel better — with personal, one-on-one service that meet your special needs. Some services offered include hats and scarves, wigs for hair loss, clinical care for sensitive skin and nails, acupuncture, aromatherapy, facials, massages, yoga classes, guided meditation, exercise programs, art therapy, and support groups.

Palliative Care
Palliative care is a team-based medical specialty that works with patients who have a serious illness to assist with improving their quality of life. Services provided by this team may be different at different phases of your cancer treatment. Often, palliative care is involved in the management of symptoms related to your cancer or cancer treatment. They may also assist with ensuring that cancer treatments are in line with your goals. Our Palliative Care team consists of doctors, nurse practitioners, and a nurse who works collaboratively with your oncology team, social worker, psychologist, chaplain, and other supportive services to ensure your quality of life is maximized throughout your cancer treatment course.