Everson Laboratory
Location
Health Research Center
H4145
General Interests
Physiology, Endocrinology, Metabolism
Research Areas
Intervening in mild traumatic brain injury to improve outcomes. Our laboratory is investigating practical interventions that may be implemented in the field to improve outcomes after mild traumatic brain injury (mTBI). Each intervention under study – sleep augmentation, sleep restriction, caffeine, and sedation – is known to profoundly affect cerebral blood flow and metabolism, which are integral to injury sequelae. These interventions are being evaluated for changes to the extent and course of brain injury (i.e., local coherence of brain neural activity, functional brain connectivity, and microstructural disturbances) and for changes to hormonal and behavioral co-morbidities in mTBI. The results will provide basic proof of concept for practical and low-cost means to improve mTBI outcomes during acute and subacute postinjury intervals.
This initiative is supported by a grant awarded by the U.S. Army Medical Research & Development Command, Department of Defense. Collaborators include Drs. Brian Stemper and Matthew Budde, Department of Neurosurgery; Dr. Aniko Szabo, Institute for Health & Humanity; and Dr. Thomas Hammeke (retired), Department of Psychiatry and Behavioral Medicine.
Deconstructing sleep disruption as a major risk factor for relapse in opioid use. The threat of relapse to opioid use is severe and unrelenting: 40-60% of individuals who misuse or become addicted to opioids relapse weeks or months after opioid withdrawal. Profound sleep disturbances during abstinence have long been suspected of perpetuating vulnerability to relapse. Our laboratory has shown that persistent sleep disruption dysregulates the hypothalamic-pituitary-adrenal (HPA) axis—a likely biological basis of vulnerability. Therefore, we are interrogating the HPA axis to isolate the mechanism that may be maintained in a dysregulated state by persistent sleep restriction during opioid abstinence. Furthermore, two clinically relevant approaches to situations where too little or too much HPA-axis output is suspected will be tested for treatment efficacy. The functional outcome measure will be the degree of mitigation of opioid drug seeking. Characterization of vulnerable phenotypes will include stress-induced changes glucocorticoids, pain sensitivity, and responses to novel environments which may predict vulnerability.
This is a multi-principal investigator project with Dr. Everson, Dr. Christopher Olsen, Department of Pharmacology & Toxicology and Dr. Hershel Raff, Departments of Medicine, Physiology and Surgery. Collaborating scientists include Dr. Aniko Szabo in the Institute for Health & Humanity and Dr. Cheryl Stucky in the Department of Cell Biology, Neurobiology & Anatomy. This project is supported by a grant award from the National Institutes of Health HEAL (Helping to End Addiction Long-Term) Initiative.
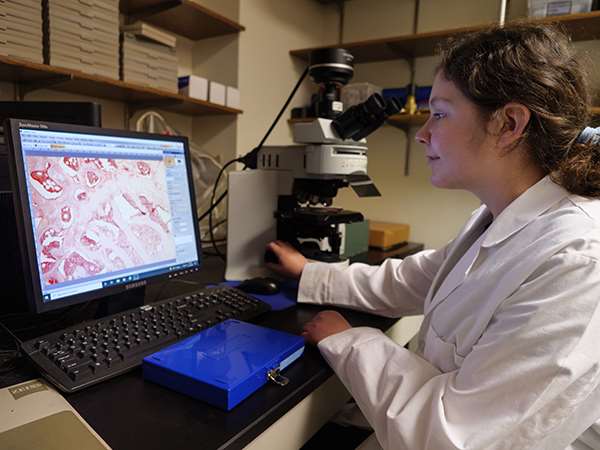
Current Members

Lance Baren
Research Technologist I

Taylor Venden
Research Technologist I
Recent Publications
-
(Everson CA, Szabo A, Olsen CM, Glaeser BL, Raff H.) Sleep. 2025 Sep 09;48(9) PMID: 40253577 PMCID: PMC12417021 SCOPUS ID: 2-s2.0-105015520801 04/20/2025
-
(Everson CA, Szabo A, Plyer C, Hammeke TA, Stemper BD, Budde MD.) Exp Neurol. 2024 Nov;381:114928 PMID: 39168169 SCOPUS ID: 2-s2.0-85201764724 08/22/2024
-
(Everson CA, Szabo A, Plyer C, Hammeke TA, Stemper BD, Budde MD.) Exp Neurol. 2024 Feb;372:114620 PMID: 38029810 SCOPUS ID: 2-s2.0-85179070318 11/30/2023
-
(Olsen CM, Glaeser BL, Szabo A, Raff H, Everson CA.) Physiol Behav. 2023 Dec 01;272:114372 PMID: 37805135 PMCID: PMC10841994 SCOPUS ID: 2-s2.0-85173957688 10/08/2023
-
(Raff H, Glaeser BL, Szabo A, Olsen CM, Everson CA.) Stress. 2023 Jan;26(1):2185864 PMID: 36856367 PMCID: PMC10339708 SCOPUS ID: 2-s2.0-85150079770 03/02/2023
-
The importance of the circadian system & sleep for bone health.
(Swanson CM, Kohrt WM, Buxton OM, Everson CA, Wright KP Jr, Orwoll ES, Shea SA.) Metabolism. 2018 Jul;84:28-43 PMID: 29229227 PMCID: PMC5994176 SCOPUS ID: 2-s2.0-85040451185 12/13/2017
-
Cell injury and repair resulting from sleep loss and sleep recovery in laboratory rats.
(Everson CA, Henchen CJ, Szabo A, Hogg N.) Sleep. 2014 Dec 01;37(12):1929-40 PMID: 25325492 PMCID: PMC4548518 SCOPUS ID: 2-s2.0-84914093940 10/18/2014
-
Chronically inadequate sleep results in abnormal bone formation and abnormal bone marrow in rats.
(Everson CA, Folley AE, Toth JM.) Exp Biol Med (Maywood). 2012 Sep;237(9):1101-9 PMID: 22946089 PMCID: PMC3939802 SCOPUS ID: 2-s2.0-84866443267 09/05/2012
-
(Everson CA, Szabo A.) PLoS One. 2011;6(8):e22987 PMID: 21853062 PMCID: PMC3154920 SCOPUS ID: 2-s2.0-80051644490 08/20/2011
-
(Everson CA, Szabo A.) Am J Physiol Regul Integr Comp Physiol. 2009 Nov;297(5):R1430-40 PMID: 19692662 PMCID: PMC2777777 SCOPUS ID: 2-s2.0-70449672782 08/21/2009
-
(Everson CA, Thalacker CD, Hogg N.) Am J Physiol Regul Integr Comp Physiol. 2008 Dec;295(6):R2067-74 PMID: 18945949 PMCID: PMC2685300 SCOPUS ID: 2-s2.0-57749108208 10/24/2008
-
(Everson CA.) Am J Physiol Regul Integr Comp Physiol. 2005 Oct;289(4):R1054-63 PMID: 15947073 SCOPUS ID: 2-s2.0-25844438769 06/11/2005

